Femoral shaft fractures are usually high-energy fractures. They may be associated with significant blood loss into the thigh compartments (2-3 units if closed, more if open or bilateral). In addition, associated injuries (pelvic fractures, femoral neck fractures, 50% incidence of ipsilateral meniscal pathology) may alter the treatment of prognosis.
Clinically, these patients will present with pain, deformity, shortening, swelling. Based on the mechanism, they should receive a full trauma evaluation and a careful screening for other injuries. A complete neurovascular exam both before and after the application of traction or immobilization should be documented. An exam for ligamentous stability of the knee may be deferred until after stabilization of the fracture, but obvious ligamentous instability may preclude through-knee traction.
Anatomy –
Femoral shaft fractures are defined as fractures of the femoral diaphysis from 5 cm distal to the lesser trochanter to 5 cm proximal to the adductor tubercle. The femoral shaft in this area is a tubular structure with a gentle anterior bow, flaring into the metaphysis proximally and distally. Axially, the intramedullary canal sits distal to the piriformis fossa.
The major source of blood supply to the femoral diaphysis is a single nutrient vessel that is supplied by the first or second branch from the profunda femoris. This nutrient vessel pierces the cortex in the proximal ½ of the diaphysis near the linea aspera posteriorly and supplies the blood for the inner 2/3 to ¾ of the cortex, while the periosteal vessels supply the outer 1/3 to ¼ of the cortex. After fracture, the endosteal supply is disrupted, and the periosteal vessels proliferate and assume the dominant role in supplying the cortex.
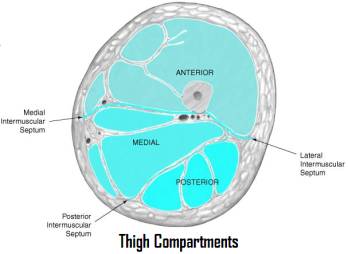
There are three compartments of the thigh. The anterior compartment contains the quadriceps femoris, sartorius, iliacus, psoas, pectineus, femoral vein, artery, and nerve, and the lateral femoral cutaneous nerve. The medial compartment contains the gracilis, the adductors (longus, brevis, magnus), the obturator externus, the obturator vein, artery, and nerve, and the profunda femoris artery and vein. The posterior compartment contains the semitendinosis, semimembranosis, biceps femoris, portions of adductor magnus, sciatic nerve, posterior femoral cutaneous nerve, and branches of the profunda femoris nerve. Compartment syndrome in the thigh is rare; however, it may be associated with high-energy trauma and prolonged traction on the fracture table with the use of a perineal post.
Radiographs and Classification –
Radiographic evaluation should include AP and lateral views of the femur, as well as dedicated hip (2-5% incidence of femoral neck fracture) and knee films.
There is no universally accepted classification for femoral shaft fractures. They are described by location (proximal, middle, distal thirds), pattern (transverse, oblique, spiral), and degree of comminution (butterfly fragments, segmental comminution, % of intact cortex abutting).
Treatment –
Since the pioneering work by Küntscher in the 1930s and 40s, femoral shaft fractures are treated primarily by intramedullary fixation. Intramedullary nails have many biologic and biomechanical advantages over other treatments, leading to very high (95-99%) fracture union rates and early mobilization, even in open fractures. Traction treatment, once standard of care, has largely been abandoned due to high morbidity and mortality associated with its use. Cast bracing, although inferior to IM nailing in results, may have indications with highly comminuted midshaft/distal third fractures in medically unstable patients. External fixation may be used as a temporizing measure or rarely as definitive fixation in polytrauma patients who cannot tolerate open surgery or in severely contaminated or compromised open wounds (grade IIIB or C). Compression plating has a role in fractures with proximal or distal metaphyseal extension (ipsilateral neck, intertroch, supracondylar fracture), or when arterial injury necessitates dissection of the thigh and exposure of the cortex.

