A. Midshaft Radius and Ulna Fractures
Fractures of the shaft of the radius and ulna usually occur from a direct blow to the arm, as in a motor vehicle accident, motorcycle accident, assault, gunshot, or sports-related, or in a fall from a height. Fracture of one or both of the radius or ulna may be seen, along with various patterns of dislocation.
Anatomy –
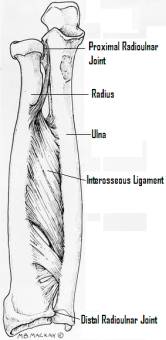
The forearm is composed of the relatively straight ulna and the bowed radius. These bones are in contact proximally at the proximal radioulnar joint, where they are bound by the elbow joint capsule and the annular ligament, which wraps around the radial neck. Distally, they contact each other at the distal radioulnar joint (DRUJ), which is stabilized by the triangular fibrocartilage complex (TFCC). The interosseous ligament or membrane runs between the bones, and helps maintain their relative positions, with a strong central band providing the majority of the support.
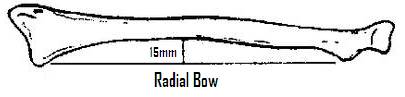
The radius bows laterally approximately 15mm at its midpoint. This bow is important in allowing the radius to rotate around the ulna in pronation and supination.
On exam, pain and deformity are usually obvious. Tenderness to palpation and crepitus may be elicited, but are usually unnecessary for diagnosis. A careful neurovascular exam should be documented, and repeat neurovascular exams are important, as these injuries are susceptible to compartment syndrome. AP and lateral radiographs of the forearm, wrist and elbow should be obtained; while the fractures will usually be evident, subtle malalignment of the DRUJ and radial head should be evaluated. Radiographs of the opposite forearm may be useful in evaluating alignment. CT may be helpful in evaluating the DRUJ.
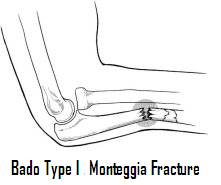

Fractures are described by location within the bone (divided into thirds), displacement, angulation, and pattern. Eponyms are associated with various fracture patterns: nightstick fractures refer to isolated ulnar shaft fractures; Monteggia fractures are ulnar shaft fractures with radial head dislocation; Galeazzi fractures are distal third radius fractures with dislocation of the DRUJ.
Treatment –
Most fractures of the radius and ulna in adults are displaced, and open reduction and internal fixation is the treatment of choice. Closed reduction is reserved for those with contraindications to surgical treatment, and unsatisfactory results may be expected up to 71% of the time. External fixators may be indicated for contaminated open fractures and fractures with significant soft-tissue compromise. Intramedullary nailing is rarely used in adults. Anatomic reduction of the fracture is usually successful in reducing the dislocations associated with Galleazi or Monteggia fractures. If the joint is not reducible, fracture reduction should be reassessed; soft-tissue interposition may require open reduction. If the DRUJ is unstable after anatomic reduction, a radioulnar pin may be used to hold reduction.
Nightstick fractures are significantly more stable than both-bone forearm fractures. If non-displaced (<10 degrees angulation, less than 50% translation), they may be splinted initially and treated in a functional brace for 4 to 6 weeks. Displaced or open fractures should be treated by ORIF.
B. Elbow Fractures and Dislocations
Anatomy –
The elbow is composed of the ulnohumeral, radiohumeral (or radiocapitellar), and proximal radioulnar articulations. The stability of the elbow relies on osseous, ligamentous, and muscular structures. The olecronon and coronoid processes resist anterior and posterior forces respectively as part of the greater sigmoid (semilunar) notch of the ulna surrounding the trochlea. In extremes of flexion and extension, these structures lock into their fossae, providing additional stability. The radiacapitellar articulation provides additional stability to valgus stresses as it widens the base of the joint, and by tensioning the lateral ligaments, provides varus stability as well. The anterior band of the medial collateral ligament inserts distally and medially to the coronoid and provides up to one-half of the medial stability of the elbow. The lateral ligamentous complex inserts on the annular ligament, and resists lateral and posteriolateral rotational instability. The biceps, brachialis, triceps, supinator, extensor carpi ulnaris, and extensor origin provide some measure of stability to the elbow.
Olecranon Fractures –
The olecranon is a subcuataneous structure, making it succeptible to direct trauma from a fall on a flexed elbow. Avulsion of the posterior portion of the olecranon from the pull of the triceps during a fall on a partially flexed elbow may occur as well. The elbow will be tender to palpation with a large hemorrhagic effusion, as this is an intraarticular fracture. The fracture may be palpated below the skin if it is widely displaced. Testing of the competence of the triceps mechanism against gravity is important, as is a complete neurovascular exam.
AP and lateral plain films should be obtained. The lateral will provide information as to the continuity of the joint surface, degree of displacement and comminution. The AP will help identify angulation and associated radial head fractures.

Nonoperative treatment of olecranon fractures is appropriate in non-displaced (displaced less than 2mm), stable (no change in position when extended and flexed to 90 degrees) fractures. Closed treatment consists of an above-elbow cast with the arm flexed to 90 degrees for 3-4 weeks and protected range of motion for 2-4 more weeks, avoiding flexion past 90 degrees. Frequent radiographs should be obtained to ensure that the fracture does not displace late.
ORIF should be undertaken when the displacement of the fracture is greater than 2mm or when the reduction cannot be maintained with the elbow at 90 degrees. A combination of tension band wiring, plate fixation, and lag screws may be used, and excision of small or comminuted fragments may rarely be indicated.
Radial Head Fractures –
The radial head serves as a stabilizer to the elbow with valgus forces. In addition, it serves as the primary restraint to proximal migration of the radius, working in concert with the interosseous ligament and the triangular fibrocartilage complex (TFCC) of the distal radioulnar joint (DRUJ).
Radial head fractures may occur with a valgus loading mechanism or axial loading through a fully extended and supinated forearm. Clinically, this may be evident as tenderness to palpation over the radial head, pain with range of motion (including supination, pronation, and valgus loading), swelling over the posterio-lateral aspect of the elbow. Swelling of the forearm distally and tenderness over the wrist should be noted, as they may signify damage to the interosseous ligament and TFCC/DRUJ. AP, lateral, and oblique radiographs should be obtained initially, although if a posterior fat pad sign is present without visible fracture or for evaluation of intraarticular step-off and pre-operative planning, specialized radial head views or CT scan may be helpful.
The Mason classification system is based on degree of radial head involvement and displacement. Type I fractures are small or marginal fractures with minimal displacement (<2mm). Type II fractures are marginal fractures with displacement >2mm, and type III fractures are highly comminuted fractures.
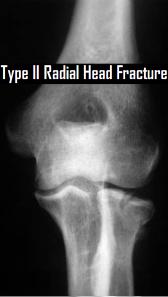
Treatment of radial head fractures is dependent on fracture characteristics as well as the associated injuries in the surrounding tissues. Type I fractures may be treated with a sling with or without a short (3-4 days) course of immobilization. Active forearm rotation is begun immediately, and range of motion should steadily improve over 2-3 months.
Type II fractures may be treated several ways. If there is no mechanical block and displacement is minimal, then the fracture may be treated closed, similar to a type I. If there is a mechanical block, crepitus, or joint incongruity, surgical treatment is indicated. ORIF should be considered in young, high-demand patients. In low-demand patients, partial or complete radial head excision may be considered. With evidence of interosseous ligament or DRUJ injury, radial head excision may lead to proximal migration of the radius and DRUJ symptoms, so ORIF versus prosthetic replacement of the radial head should be considered.
In type III fractures, the radial head is not repairable by definition. Therefore, radial head excision is recommended. Prosthetic replacement is recommended if there is evidence of IOL or DRUJ symptoms, or concomitant dislocation.
Elbow Dislocations –
Elbow or ulnohumeral dislocations may be posterior, anterior, medial, lateral, or divergent, based on the position of the ulna relative to the humerus. Posterior dislocation is the most common, caused by a fall on an outstretched hand with hyperextension and rotation leading to failure of the anterior capsule and medial collateral ligaments. Anterior dislocation may be caused by a fall on a flexed forearm. Fractures of the distal humerus, coronoid process, olecranon, and humeral head may occur and affect the stability of the reduction.
A careful assessment of neurovascular status pre- and post-reduction should be documented. Nerve deficit present both pre- and post-reduction may be due to traction injury, and should be observed for a period of time (3-6 months). Any loss of nerve or arterial function following reduction requires exploration for entrapment. Prolonged ischemia may require fasciotomies to prevent compartment syndrome.
Closed reduction with longitudinal traction on the forearm and counter-traction on the anterior humerus should be attempted for posterior dislocations. Anterior dislocations should be treated with posterior and downward pressure on the forearm and counter-pressure on the posterior aspect of the distal humerus. Open reduction may be indicated if closed reduction fails, and ORIF of concomitant fractures should be undertaken as required to provide stability to the elbow. Repair of the collateral ligaments is not indicated. Range of motion is initiated within the first week.
C. Distal Humerus Fractures
Anatomy –
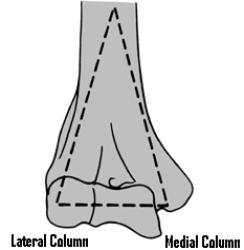
The distal humerus at the metaphyseal flare divides into medial and lateral columns, connected by an articular “tie-arch”, composed of the trochlea and capitellum. These columns pass around an area that thins to a cortical shell of bone only millimeters thick at the coronoid and olecranon fossae. The medial column terminates at the non-articular medial condyle, while the lateral column terminates at the capitellum. The medial epicondyle is the site of origin of the medial collateral ligaments of the elbow and is closely associated with the ulnar nerve.
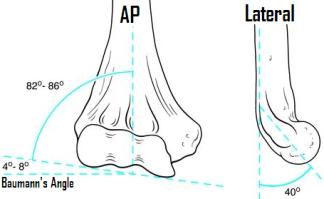
The articular surface of the humerus makes a valgus angle of 4-8 degrees from the perpendicular, called Baumann’s angle or the “carrying angle” of the elbow. The distal humerus projects anteriorly from the axis of the humerus at approximately 40 degrees, so that a line continued from the anterior cortex of the humeral shaft bisects the capitellum on the lateral projection.
Diagnosis –
The mechanism of injury in distal humerus fractures is typically a load on an elbow flexed beyond 90 degrees. Studies suggest that flexion less than 90 degrees results in olecranon fractures. On exam, the patient will have pain, swelling, and restricted range of motion. A neurovascular exam, with special attention to the ulnar nerve, should be documented.
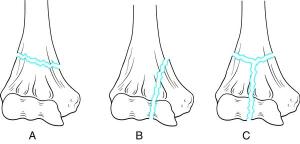
Radiographs should include AP and lateral views of the elbow. In displaced fractures, gentle traction views may improve visualization of the fracture. The Orthopaedic Trauma Association classification is typically used, dividing distal humerus fractures into Type A (non-articular), Type B (partial articular or unicondylar, with part of the articular surface in continuity with the shaft), and Type C (bicondylar or T-type, with no articular surface in continuity with the shaft). Type C fractures are further subdivided into C1 (no comminution), C2 (non-articular comminution), and C3 (articular comminution).
Distal humerus fractures are generally unstable fractures. Treatment is primarily ORIF, with plating of the involved columns (medial and/or lateral) and anatomic reduction of the joint surface. Care must be taken to avoid placing a screw into the olecranon or coronoid fossae. Open fractures and fractures in severely debilitated or osteoporotic patients may preclude ORIF, in which case elbow-spanning external fixation or traction using an olecranon pin for 2-3 weeks followed by protected range of motion may be used. Closed treatment, with the elbow flexed beyond 90 degrees and relying on ligamentotaxis for reduction, is also described.
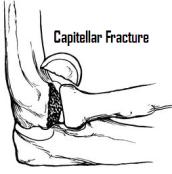
Coronal capitellar fractures that do not compromise the lateral column may also be seen. These fractures may be stable, and if non-displaced may be treated closed with 2-3 weeks of splinting followed by protected range of motion. If displaced, they require ORIF.
D. Humeral Shaft Fractures
Anatomy –
The shaft of the humerus is defined as the area between the pectoralis major insertion proximally and the supracondylar ridge distally. The deltoid inserts laterally just proximal to the midshaft and is a major deforming force in shaft fractures. The humerus is round in cross-section proximally, and assumes a triangular shape distally. The intramedullary canal is wide proximally and begins to narrow approximately 3cm, and is completely filled 1.5cm, proximal to the olecranon fossa.
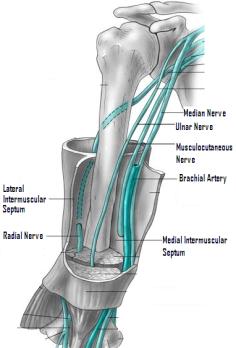
The arm is divided into anterior and posterior compartments by fascial septae. The posterior compartment contains the triceps, and proximally the radial nerve enters the posterior compartment and lies deep between the lateral and long heads of the triceps. While it is protected by muscle throughout much of its course, the radial nerve is vulnerable to injury as it swings laterally in the spiral groove of the humerus in the middle third and in the distal third, where it pierces the lateral intramuscular septum and passes into the anterior compartment. The anterior compartment contains the biceps brachii, brachialis, and coracobrachialis, as well as the brachial artery, the musculocutaneous nerve, the median nerve, the ulnar nerve proximally and the radial nerve distally. Distally, the ulnar nerve pierces the medial intramuscular septum to pass into the posterior compartment.
Diagnosis –
Fractures of the humeral shaft may occur from a direct blow (creating a transverse fracture pattern) or from an indirect twisting mechanism (creating a spiral oblique pattern. Pain and deformity will be evident, as well as crepitus. A careful neurovascular exam should be documented, with attention paid to radial nerve function, as it is most at risk. Soft tissues should be inspected for a fracture opening.
AP and lateral radiographs of the humerus, as well as shoulder and elbow, should be obtained. Description of the fracture is based on pattern, location, angulation, and displacement.
Treatment –
Closed treatment is the standard for most humeral shaft fractures, even when displaced and angulated. The mobility of the shoulder and elbow, the abundant muscular coverage, and the fact that the humerus is not used for ambulation makes a large degree of angulation (15 degrees), rotation, displacement, and shortening much better tolerated in the humerus than in other long bones. Sling and swathe techniques provide for patient comfort but little reduction. Hanging arm casts, coaptation splints, and functional bracing rely on gravity to achieve adequate reduction, with the arm supported distally in the forearm and the elbow allowed to hang free. Range of motion of the shoulder and elbow should be initiated as soon as pain allows, and protection should continue for 8 weeks.

Operative treatment of humerus fractures is indicated in selected cases. Pathologic fractures, fractures associated with brachial artery or brachial plexus injury, segmental humeral fractures and multitrauma patients with multiple long-bone fractures, spinal fractures, or floating elbow, bilateral upper extremity fractures, or injury requiring crutches may be candidates for primary operative treatment. Patients who fail closed treatment due to failure to maintain adequate reduction may also be treated operatively. ORIF with compression plating provides anatomic reduction and the opportunity to visualize the fracture site in the setting of nerve or arterial injury. Intramedullary nailing, with either flexible nails or small diameter, unreamed interlocking nails may also be effective. Open fractures may be treated by irrigation and debridement and external fixation.

