Describing Fractures
To adequately describe an injury to someone who can’t see the patient or the radiographs, it is important to understand orthopedic terminology and use it correctly to create a coherent and succinct picture. Following an accepted framework, it is possible to quickly break down a complex injury to its clinically relevant elements and communicate these to a sleepy attending or grumpy consulting orthopedic surgeon. The important elements are location, fracture (or dislocation) type, translation or displacement, angulation, and a description of the soft tissue surrounding the injury.
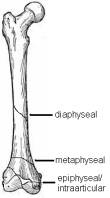
Location
Beyond describing which bone is involved, describing exactly which part of the bone is involved affects treatment and prognosis. Intraarticular, metaphyseal, or diaphyseal are good paces to start, and then narrow it down further from there.
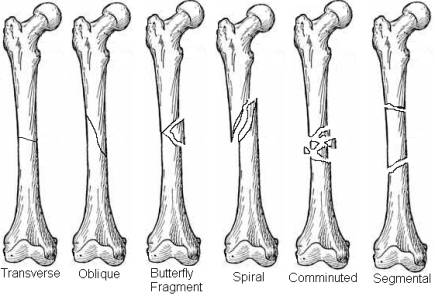
Fracture Types
The orientation of the primary fracture line, the presence of secondary fractures, butterfly fragments, or significant comminution, as well as derangements of nearby joints (fracture-dislocations) should be described.
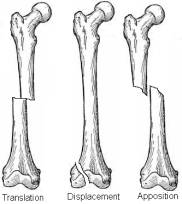
Translation or Displacement
Translation is the degree of displacement of the two fracture ends in a metaphyseal or diaphyseal fracture. It is given as a percentage of the diameter of the bone and may be present on more than one view. In an intraarticular fracture, it is more appropriate to discuss displacement of the fracture fragments, described in millimeters.
Angulation
Used to describe diaphyseal or metaphyseal fractures, angulation is expressed in degrees and described by the direction of the apex of the angle. Angulation may be present on more than one view.

Soft Tissue
Soft tissue injury has a significant effect on the treatment and prognosis of an injury. Open fractures require urgent irrigation and debridement, and may significantly affect the timing and choice of operative treatment. Significant traction injuries (in which the skin and dermis are avulsed from the underlying blood supply of the fascia), significant ecchymosis, or even abrasions may compromise wound healing should operative treatment involve violating these areas. Compromise of neurovascular status as well as the presence of a compartment syndrome should be factored into early decision making.
Modified Gustilo-Anderson Classification of Open Fractures
| Type | Wound | Soft-Tissue Injury | Bone Injury | |
| I | < 1 cm long | Clean | Minimal | Simple, minimal comminution |
| II | > 1 cm long | Moderate | Moderate, some muscle damage | Moderate comminution |
| III* | ||||
| A | > 10 cm long | High | Severe with crushing | Usually comminuted; Soft-tissue coverage of bone possible |
| B | > 10 cm long | High | Very severe loss of coverage | Bone coverage poor; usually requires soft-tissue reconstruction |
| C | > 10 cm long | High | Very severe loss of coverage plus vascular injury requiring repair | Bone coverage poor; usually requires soft-tissue reconstruction |
* Segmental fractures, farmyard injuries, fractures occurring in a highly contaminated environment shotgun wounds, or high-velocity gunshot wounds automatically result in classification as a type III open fracture. (Chapman, M.W.: The Role of Intramedullary Fixation in Open Fractures, Clin. Orthop., 212:27, 1986.)
Basics of Orthopedic Treatment
Treatment of orthopedic injuries can be broken down into operative and non-operative categories. Non-operative treatments include such modalities as traction, splinting, casting, functional bracing, and observation (no intervention). Operative treatments may include open reduction and internal fixation (ORIF), intramedullary nailing, external fixation, primary arthroplasty, or amputation.
Non-operative Treatments
Non-operative treatment modalities are appropriate in closed, minimally or non-displaced, stable fractures. While this is a good rule of thumb, it does not always hold true. Some widely displaced fractures (midshaft radius) can be effectively treated closed, while many non-displaced fractures may be unsuitable for closed treatment. Finally, when the goals of open treatment cannot be met (improved alignment, early range of motion) due to the extent of the injury, the bone quality, or the patient’s health, non-operative modalities are indicated.
Operative Treatment
Operating on a fracture does not make it heal faster; rather, by draining away pro-inflammatory cytokines and stripping away the periosteal blood supply, surgery frequently makes fractures heal much more slowly. What surgery does do is allow the surgeon to better control the deforming forces acting on a fracture that lead to malunion, provide anatomic reduction of articular surfaces, and allow earlier range of motion in the affected extremity.
ORIF – Open Reduction refers to making an incision to directly visualize the fracture site and anatomically reducing the fracture fragments. Internal Fixation refers to holding these fragments in anatomic alignment using a variety of implants (generally, plates and screws). Usually used in closed fractures due to the risk of implant contamination.
Intramedullary Nailing – Used primarily in diaphyseal fractures of long bones, intramedullary nailing is placement of a long metal nail of varying diameter through the intramedullary canal from end to end of a bone, crossing the fracture site and providing stability. Normally, this does not necessitate opening of the fracture site. This technique may be used in closed and some open fractures. Frequently nailed bones include the femur, tibia, humerus, and ulna.
External Fixation – In external fixation, transcutaneous pins or wires hold fracture ends and allow them to be manipulated from an outside frame. This may provide indirect reduction (without opening the fracture site) as well as provide traction. An ex-fix is frequently used when extensive soft tissue injury and wound contamination is a concern.
Arthroplasty and Amputation – Some injuries are too severe to contemplate salvaging a limb or joint. In other cases, experience tells us that the fracture will not heal well with operative or non-operative treatment. In these cases arthroplasty or amputation are valid options.
Compartment Syndrome
One of the few true orthopedic emergencies, compartment syndrome deserves mention. Compartment syndrome occurs when the pressure in an enclosed space (such as a fascial envelope) increases to the point that it begins to restrict capillary blood perfusion and compromises tissue viability. This may occur when volume within the space increases (such as hemorrhage or edema) or the size of the space decreases (such as a tight circumferential cast). Prolonged ischemia affects nerve and muscle function and may progress to irreversible damage.
Compartment syndrome is a clinical diagnosis. The classic “five Ps of compartment syndrome” (sometimes six) are: pain (out of proportion to the injury, with passive stretch), pallor, pulselessness, paresthesias, paralysis, (and poikilothermia – coldness). Paresthesias and pain with passive stretch are the first two signs that will develop; pallor and pulselessness may not be seen until very late in the course.
In unconscious patients, compartment pressures may be measured to determine risk for compartment syndrome. Do not measure pressures in conscious patients. The classic guideline of an absolute compartment pressure of 30mmHg as diagnostic for compartment syndrome has largely been replaced by a criteria of a compartment pressure within 30mmHg of the diastolic blood pressure.
Diagnosis of compartment syndrome leads to emergent fasciotomies. Experimental studies have shown irreversible damage to nerves and muscles occurs within eight hours of onset. The risk of compartment syndrome extends for 24 hours following injury or surgery.

