Fracture of the tibial diaphysis (with or without fracture of the tibia) is the most common long-bone injury. It occurs in a bimodal distribution, with the highest risk in young males ages 15-19, gradually decreasing in incidence through middle age, with a second peak in elderly (osteoporotic) men and women. Five common mechanisms of tibial shaft fractures include falls, sports injuries (including boot-top fractures seen in skiers), direct blows, MVAs, and gunshots. As almost ¼ of tibial fractures are open fractures, the physical examination should include a careful evaluation and description of the extent of any soft tissue injury; likewise, given the high incidence of compartment syndrome and the susceptibility to injury of the tethered common peroneal nerve and popliteal artery, a carful neurovascular exam must be documented.
Fibula shaft fractures may occur in conjunction with tibia fractures through any of the above mechanisms. When they occur in the absence of a tibial injury, the mechanism is usually either a direct blow or associated with a twisting injury of the ankle (as in a maisonnueve fx).
Anatomy –
The anatomy of the tibia predisposes it to certain types of injury and complicates the treatment of fractures. The anterior-medial border of the tibia is directly subcutaneous, making it susceptible to fracture a direct blow is sustained. Furthermore, this makes the tibia more prone to open fractures (23.5% of tibial fractures are open) and makes the blood supply to both the tibia itself and the overlying skin tenuous in the face of trauma and surgery. From the proximal metaphyseal flare, the tibia narrows gradually to be narrowest in diameter at the middle-distal 1/3 junction. This region is especially susceptible to twisting injuries resulting in spiral fractures.
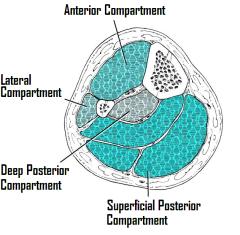
The leg is divided into four musculofascial compartments. The anterior compartment contains the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius muscles, the anterior tibial artery, and the deep peroneal nerve. The lateral compartment contains the peroneus longus and peroneus brevis muscles, and the superficial peroneal nerve. The superficial posterior compartment contains the gastrocnemius, soleus, and plantaris muscles, and the deep posterior compartment contains the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles, and the posterior tibial artery and nerve. The leg is particularly susceptible to compartment syndrome (4.7% in closed fractures, 3.3% in open), especially the anterior and deep posterior compartments.
Radiographs –
The radiographic evaluation of the tibia and fibula should include AP and lateral plain films of the leg as well as the ankle and knee. There is no widely accepted classification system for describing tibia fractures; rather, they are described by radiographic appearance in terms of fracture location, pattern, displacement, comminution, and extension into adjacent joints, as well as the condition of the fibula.
Treatment –
Non-operative treatment of tibial fractures with long-leg casts, patellar-tendon-bearing casts, or functional bracing has limited indications. These treatments may be undertaken in young patients with closed, low-energy, non- or minimally-displaced fractures, or in patients with low functional demands or co-morbidities precluding surgery. High incidence of malunion (as high as 50%) and hindfoot stiffness (25-45%) limit the use of these techniques.
Intramedullary nailing is the treatment of choice for almost all tibial shaft fractures. IM nails give the best results in terms of rate of union, time to union, and complications. There is minimal insult to the compromised soft tissue and the implant is not subcutaneous. Studies have shown nailing to be effective in open fractures, even severely contaminated fractures. Reamed nailing versus unreamed nailing continues to be debated in the literature, but reamed nailing appears to be more effective in most situations, with the possible exception being very contaminated open fractures. IM nailing may be undertaken for fractures throughout the tibial diaphysis to within 2cm of the tibial plafond, although very proximal fractures may tend to mal-unite, necessitating “blocking screws” to maintain alignment. Knee pain is a common complication with IM nailing (occurring in ~50%), which is usually mild or moderate and resolves or improves with removal of the nail.
Plating of tibial fractures has fallen out of favor due to the complications associated with the insult to the compromised tissues surrounding the fracture. It remains a useful technique in cases where there are significant articular or peri-articular fractures in association with tibial shaft fractures.
External fixation of tibial fractures plays a role in the treatment of multiple extremity trauma when the patient cannot tolerate the surgery time that definitive treatment would entail. It may also play a role in treatment of severely contaminated Gustillo IIIb or c fractures, as definitive treatment of with secondary conversion to IM nail at a later date.
Amputation may be required primarily or secondarily in 17% of Gustillo IIIb fractures, and as many as 85% in IIIc fractures.
Isolated fibula fractures occurring in the presence of knee or ankle injuries should be treated as appropriate for the associated injury. True isolated fibula fracture may be treated symptomatically with early weight-bearing in a walking boot or short leg cast.
Complications –
Tibia fractures are associated with a high rate of complications including: non-union (defined as 9 months from surgery/injury without union AND 3 months without progression, occurring in 3-40% based on the severity of the soft-tissue injury and the treatment modality), malunions, compartment syndrome, refracture, and reflex sympathetic dystrophy.