Rotator Cuff Anatomy
The rotator cuff is composed of the tendinous portions of four muscles: the supraspinatus, infraspinatus, teres minor and the subscapularis. The rotator cuff acts as a major stabilizer to the glenohumeral joint. The cuff musculature provides dynamic stability to the glenohumeral joint, keeping the humeral head within the shallow glenoid cavity during shoulder range of motion. The innervation, major blood supply and primary action of the rotator cuff muscles are listed in Table I.
TABLE I |
|||
| Rotator Cuff | Innervation | Blood Supply | Primary Action |
| Supraspinatus | Suprascapular nerve | Suprascapular artery | Abduction |
| Infraspinatus | Suprascapular nerve | Suprascapular artery | External rotation |
| Teres Minor | Axillary nerve | Posterior humeral circumflex artery | External rotation |
| Subscapularis | Upper and lower subscapular nerves | Axillary and subscapular arteries | Internal rotation |
Impingement/Rotator Cuff Disease
Impingement is a term used to describe shoulder pain related to a decreased subacromial space with abutment of the greater tuberosity and the inferior acromion. A hooked acromial shape and formation of inferior acromion spurs are both associated with classic outlet impingement. Impingement of the rotator cuff has been classified into three stages: initial inflammation and edema (I), tendonitis (II), and tearing of the rotator cuff (III).
Classic impingement caused by a mechanical narrowing within the subacromial space usually occurs in patients around forty years and older and is rare in the younger population. However, impingement has been described in the young, athletic population, particularly in overhead athletes. This is referred to secondary impingement. The pathology of secondary impingement is related to microtrauma of the glenohumeral static restraints from repetitive activities. The injury to the shoulder static restraints increases glenohumeral translation and can cause impingement symptoms.
Rotator cuff tears, much like impingement, occur most frequently in patients over forty years old. Rotator cuff tears are multi-factorial in nature and can be caused by mechanical (impingement, overuse) or age-related (tendon degeneration, delayed healing ability, poor vascularity) pathology. It has been estimated that after the age of 40, up to 30% of patients may have a rotator cuff tear. After the age of 60, up to 80% of patients may have a rotator cuff tear. Although rare, rotator cuff tears may occur in the younger population usually secondary to a direct blow to the shoulder or repeated overhead activities.
History
Most patients with rotator cuff pathology will complain of anterior shoulder pain and difficulty with overhead activities. Patients with rotator cuff tears often complain of night pain. They may complain of stiffness and weakness as well.
Physical Exam
The physical exam of the rotator cuff should begin with inspection, palpation, evaluation of passive and active range of motion and strength testing. Inspection may reveal atrophy of the supraspinatus and infraspinatus. Often patients with rotator cuff pathology have tenderness anterior and lateral to the acromion. Active and passive range of motion is important since patients with rotator cuff tears often have decreased active motion compared to passive motion.
Isolation of infraspinatus
Isolation of supraspinatus
Gerber lift-off test
The primary function of the supraspinatus is to abduct the shoulder concurrently with the deltoid. The optimal position for isolated strength testing of the supraspinatus is at 90º of elevation and 45º of external rotation.
The infraspinatus and teres minor are primary external rotators of the shoulder. The optimal position for infraspinatus strength testing is at 0º elevation and 45º internal rotation.
The subscapularis is primarily an internal rotator of the shoulder. One method of isolating the subscapularis is by performing the lift-off test. The lift-off test is performed by placing the hand in the mid-lumbar region and the patient is asked to lift the hand off the back. Weakness of the subscapularis is noted with the inability to bring the hand away from the back. The belly press test is another way to assess subscapularis function.
Neer Test
Hawkins Test
The Neer and Hawkins tests are both used to diagnose shoulder impingement. Both tests decrease the available subacromial space by bringing the greater tuberosity of the humerus into closer proximity to the acromion. The Neer test is performed by elevating the arm while rotated in internal rotation. The Hawkins test is performed with the shoulder at 90º forward flexion, adducted across the chest and internally rotated. Both tests are positive when pain is elicited with the described motions.
Imaging
Imaging begins with radiographs of the shoulder. The typical shoulder series includes at least an anteroposterior, scapular Y, and axillary radiograph. With large rotator cuff tears the humerus may be “high riding” with a decreased acromiohumeral distance. Degenerative changes in the glenohumeral joint may also be seen in chronic cuff tears. The axillary image is used to evaluate the glenohumeral joint space and the scapular Y view is primarily used to assess the acromion morphology.
Scapular Y view with hooked acromion

MRI with rotator cuff tear
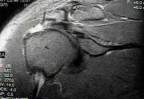
Imaging of the rotator cuff musculotendinous unit can be assessed by shoulder arthrogram, MRI and ultrasound. All three studies can be helpful in the assessment of rotator cuff tears.
Treatment
Treatment of shoulder impingement begins with non-operative measures. Physical therapy consisting of a stretching and strengthening program is the first line of treatment. Non-steroidal medication may be used to decrease inflammation. Cortisone injections into the subacromial space may also be used to decrease inflammation.
If conservative measures do not relieve the impingement symptoms, an acromioplasty may be performed. The anteroinferior acromion and coracoacromial ligament are removed to widen the subacromial space. Both open and arthroscopic acromioplasty techniques have been shown to be beneficial in treating impingement.
Symptomatic rotator cuff tears may be treated surgically. Partial tears of the rotator cuff are treated with debridement vs. excision and repair of the tendon. General recommendations for the treatment of partial tears are debridement for tears involving less than 50% of the tendon thickness and excision and repair for tears involving greater than 50% of the tendon thickness. Symptomatic full thickness tears should be repaired if possible. This can be done with arthroscopic or open techniques. Some massive tears cannot be fully repaired. Surgical options for massive irreparable tears are medialization of the cuff, superior transposition of the subscapularis, patching the defect with tissue or synthetic material, and latissimus transfer.

