Fracture healing and the management of fractures is field that has seen great advances in the last 30 years. To understand how these advances are employed one must understand the biology of fracture repair. Once a fracture has occurred, almost immediately changes occur to the bone and surrounding tissue. Blood vessels clot, the normal vascular architecture of the bone marrow is lost as the cells within the marrow begin to reorganize. Within 24 hours these cells will transform into polymorphic cells with an osteoblastic phenotype and begin laying down bone. At this point there are two types of bone healing, primary cortical healing and secondary fracture healing.
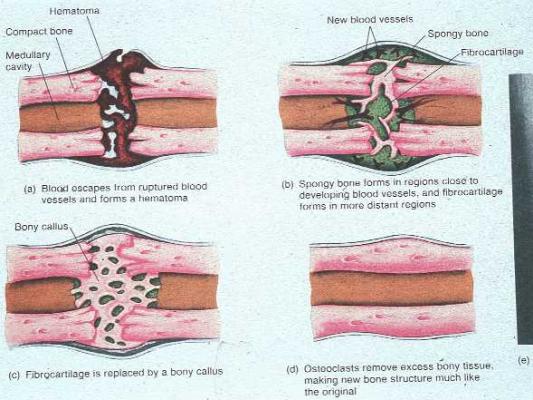
Primary cortical healing (also called direct bone healing) represents an attempt by the cortex to directly reestablish cortical continuity. This type of healing requires absolute rigid stabilization (i.e. with a metal plate) after anatomic reduction of the fracture ends. Regions where the cortical ends are in contact stabilize the other regions where small gaps are found. Within the gaps, blood vessels will infiltrate and mesenchymal cells will follow close behind to begin laying down bone after differentiating into osteoblasts. The edges of the bones on either side of the gaps become necrotic and begin to resorb. Osteoclasts at the tip of cutting cones then begin to bridge the gaps and replace the tiny callus between the bones with new osteons (Figure 24). This process is called “gap healing”. The same process simultaneously occurs at regions where the cortices are in direct contact (figure 25). When healing is complete there is no callus formation and the fracture has been replaced with new bridging osteons. Secondary fracture healing (also called indirect bone healing) involves a completely different process that relies heavily on the periosteum for healing. With the loss of the endochondral blood supply, the periosteum rapidly becomes the primary blood supply to the surrounding bone. Osteoprogenitor cells within the periosteum are mobilized and begin to form bone by processes analogous to intramembranous ossification and endochondral bone formation. Peripheral to the site of the fracture intramembranous ossification takes place to form hard callus. Cartilage is not made before the matrix is solidified and structural proteins are employed from the beginning. The hard callus has an increased diameter when compared with the normal cortex, which helps reduce the strain on the fracture site. At the fracture site, bone is formed by endochondral ossification that requires the formation of a cartilage precursor. Eventually the cartilage is replaced by much the same mechanism as described in the chapter above (See figure 6 & 7). This process is enhanced by motion at the fracture site and inhibited by rigid fixation. Intramedullary nailing of fractures provides some relative fixation at a fracture site without eliminating all motion, as in rigid fixation with a plate. The IM nail is a powerful tool because it allows the process of secondary ossification to occur at a fracture site while keeping the bones aligned. Often a substantial callus can be seen at fracture sites that have been treated with an IM nail.
Figure 24:
Demonstrates primary bone healing as well as “gap healing”.

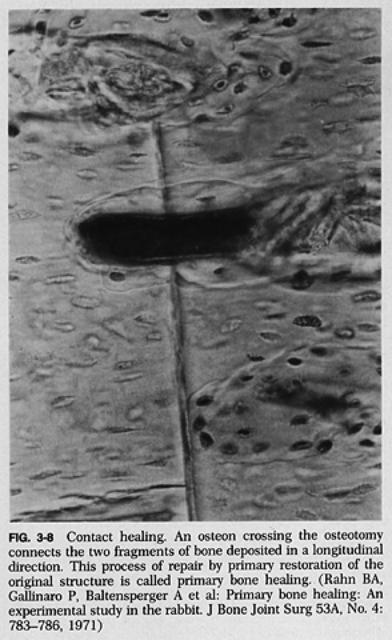
Figure:
A cutting cone crossing a fracture site; the hallmark of direct bone healing.
The processes above occur in a continuum; however, the stages of fracture healing have been roughly divided into 3 parts. Stage I, or The Inflammation Stage, begins with a localized hematoma formation and eventual organization. The hematoma helps give the fracture a small amount of stability, and more importantly, allows inflammatory cells influx to the region activated by inflammatory cytokines. The cells immediately begin to differentiate into osteoblasts and chondroblasts and begin laying down bone and cartilage. This phase will last approximately 1 month. Stage II, or The Reparative Stage, begins after about two weeks. In this stage the proteins produced by the above cells begin to consolidate into a soft callus. By 3 weeks the soft callus will be completely formed and the fracture ends will be relatively stable. Soft callus is not visible on plain film radiographs. At this point variations of intramembranous ossification & endochondral ossification occur to form a hard callus by 6 to 12 weeks. In most cases, the primary bone of the hard callus can tolerate weight bearing. While it is less stiff and has an overall lower strength than lamellar bone, its increased mass and diameter imparts sufficient stability. Stage III, the remodeling stage, begins and the callus that consists of primary bone begins to remodel to more mature secondary lamellar bone. This occurs by the same process of remodeling that normally occurs in the skeleton. It can take 3 months to several years to complete. Wolf’s law dictates that the fracture is remodeled to sufficiently manage to stresses across the fracture site. Accordingly, the callus will often thin down as the increased diameter of the callus is no longer needed to stabilize the fracture ends.
Figure 26
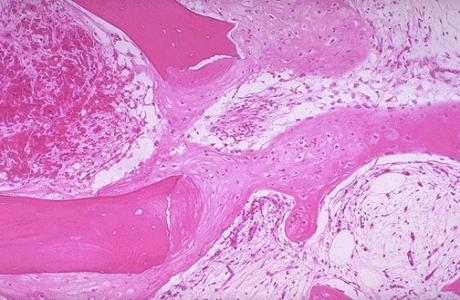
Figure 27