Hip Arthrodesis
Fusion of the hip is generally reserved for young heavy laborers with end stage DJD who would likely cause their total hip construct to rapidly deteriorate because of the excessive stresses it would experience. Surgical fusions are performed for these young adults with advanced arthritis (most commonly post traumatic DJD) who have a strong desire to return to near-normal physical activity with manual labor. The main goal of the procedure is to provide pain relief and 80% of patients with hip arthrodesis performed at relatively young age are working and satisfied with their results 20 yrs years after surgery.
Surgical prerequisites include a normal contralateral hip, ipsilateral knee, and a low back. Hip fusion increases stresses in these and other joints and cause degenerative changes 15-25 years after surgery. The most commonly involved joints in decreasing order are the lumbar spine (55-100%), ipsilateral and contralateral knees (45-68%) and contralateral hip (25-63%). It is important that patients do not have any significant cardiovascular pathology as ambulatory efficiency is decreased. Concordantly, the rate of oxygen consumption during normal gait is 32% greater than normal. The average walking speed is also reduced to 84% of normal gait velocity.
A crucial operative goal is to achieve a successful fusion. A high union rate is achieved by resecting any necrotic bone. This ensures that well-vascularized bone of the femoral head and acetabulum are in apposition and maximizes the cancellous bone surfaces in contact to provide a stable fusion mass. Rigid internal fixation should be used and when necessary iliac crest bone graft can be used to augment the fusion mass. Occasionally a vascularized muscle pedicle graft is also used.
Regardless of fixation technique, the hip should be fused in approximately 30º of flexion, 0-5º of adduction, and 0-15º of external rotation. Abduction and internal rotation should be avoided. This position is designed to minimize excessive lumbar spine motion, pelvic obliquity, and opposite knee motion which helps minimize pain in these regions. The most common complication is malposition of the arthrodesis. Chapman suggests placing the hip in 20° of flexion and neutral abduction, while placing the foot in the plane of the progression of gait to match the opposite normal side, which is usually 0° to 10° of external rotation. Excessive hip flexion may cause excessive compensatory lumbar lordosis leading to back pain and DJD. More than 10º of hip adduction or abduction may lead to varus/valgus knee instability. Other complications include nonunion, leg length discrepancy (is common and can be severe enough to require lift) and DJD or instability of surrounding joints and lumbar spine as mentioned above.
Because hip fusion is most commonly performed in young adults and the incidence of subsequent low back pain is significant, the need for conversion to total hip arthroplasty once the patient is older than 60 years of age is quite high. For that reason, use a technique that preserves the function of the hip abductor muscles with forethought for future THA conversion is key. The main indications for conversion from hip fusion to THA are: severe persistent lower back pain, pseudoarthrosis, and ipsilateral knee pain. Converted THA is very difficult and is associated with a high failure rate of 33% at 10 years. The most common reasons for failure are recurrent dislocation, loosening, and infection.
A commonly used technique for fixation employs an AO Cobra Plate. This fixation is stable but disrupts abductors and if this technique is chosen the surgeon should consider a greater trochanteric osteotomy and elevation of the abductor mechanism to preserve it for later use in THA. Another common technique is anterior plating across the anterior column of the pelvis. This is done through an extended Smith Peterson approach and does not violate the abductors.
KNEE ARTHRODESIS
The indications for knee arthrodesis are similar to those of hip arthrodesis. Additional indications for primary knee arthrodesis are a) painful ankylosis after infection, tuberculosis or trauma b) neuropathic arthropathy c) resection of malignancy about the knee with subsequent fusion and d) failed total knee replacement which is the most common indication. Better fusion rates are seen following failed normal condylar components (80%) than in failed hinged prostheses (55%) Contra-indications include 1)bilateral knee disease 2)ipsilateral ankle or hip disease 3)severe segmental bone loss and 4)contralateral leg amputation.
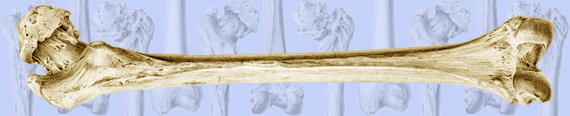
For primary arthrodesis the ideal position is 10-15 degrees flexion and 5-8 degrees valgus with 0 to 10 degrees of external rotation to match the contralateral foot. Intramedullary nailing is the preferred arthrodesis technique, especially when tumor or implant resection dose not allow for broad areas of cancellous bone to be compressed. (Figure 43) This technique is the most reliable for achieving fusion with union rates up to 100% compared to external fixation fusion rates reported at 38%. If there is active infection the procedure is done in two stages. In this scenerio an antibiotic space is place for interval to allow for clearance of the infection followed by definitive fusion. The intramedullary nail can be inserted antegrade through the piriformis fossa or retrograde through the knee joint but can be technically demanding with significant complication rates. (47) External fixation techniques allows for late adjustment of alignment as well as arthrodesis in the presence of active infection. There is minimal soft tissue destruction with this technique but the union rates are less than with IM nailing and it has a similar complication rate (20-50%).
Figure 43 Shows the IM nail technique of knee arthrodesis.