Spinal fractures occur in approximately 6% of all trauma patients, and in these patients, 15-20% have multilevel injury. Half of these patients will present with a neurological deficit.
Treatment of these injuries begins in the field. With high energy mechanism, stiff cervical collar and backboard immobilization should be initiated. These precautions should be maintained until the spine can be cleared by physical examination in the hospital and appropriate radiographs.
Physical examination –
Physical examination should proceed according to ACLS protocol. During the secondary survey, the patient is log rolled and the spine is inspected for abrasions, ecchymosis, or obvious deformity. The spine is palpated to look for pain, bogginess, or step-off between the spinous processes. Rectal examination should be done at that time, documenting sensation (light touch, pin prick, deep pressure), rectal tone (resting, voluntary contraction), and reflexes (anal wink, bulbocavernosus).
With suspected spinal injury, a careful neurologic examination is critical. The American Spine Injury Association (ASIA) has created a detailed description of the minimal elements of a neurologic assessment for patients with spinal injury. Light touch and pin prick sensation at 28 specific sensory locations bilaterally (graded 0-2, 0 – no sensation, 1 – partial diminished sensation, 2 – normal sensation) and motor function of five specific upper and five specific lower extremity muscles are graded bilaterally. From these measurements, an injury score may be generated for the patient that describes the level and extent of the neurologic injury. In practice, a less formal yet complete examination is usually done to assess the function of the specific nerve roots in question:
| Root | Sensation | Spinal Root Function Muscles | Reflex |
| C5 | Lateral Arm (Deltoid) | Deltoid/Biceps | Biceps |
| C6 | Radial Forearm/Thumb | Wrist Extensors | Brachiradialis/Biceps |
| C7 | Middle Finger | Wrist Flexors/Finger Extensors/Triceps | Triceps |
| C8 | Small finger/Ulnar Forearm | Finger Flexors/Intrinsics Intrinsics | |
| T7-T12 | Superficial Abdominal | ||
| L1 | Lateral inguinal area | Internal Oblique/Transversus Abdominis | Cremasteric (T12-L1) |
| L2 | Proximal anterior medial thigh | Hip adductors/flexors | |
| L3 | Lateral Thigh | Hip adductors/flexors | |
| L4 | Medial leg and foot | Quadriceps/Tibialis Anterior | Patellar (L3-L4) |
| L5 | 1st web space/dorsum of foot | EHL/Tibialis Posterior | |
| S1 | Lateral Foot | FHL/Gastrocsoleus/Peroneals | Achilles |
| S2 | Posterior medial leg | Anal Wink (S2-S4) | |
| S3-S4 | Peri-anal | Bulbocavernosus |
Neurologic deficit may represent nerve root or cord injury. Neurologic deficit with root injury generally involves a single level unilaterally. Cord injury may be complete (no function below the level of the lesion) or incomplete (involving specific tracts within the cord). There are four common patterns of incomplete cord injury based on the geographic location of the injury. Central cord syndrome causes a motor deficit of the upper extremities greater than the lower; recovery occurs in 75%. Anterior cord syndrome spares dorsal column function (vibration, proprioception, light touch), but causes complete motor loss below the level of the lesion; recovery is only 10%. Posterior cord syndrome affects the dorsal columns and is relatively uncommon. Brown-Sequard is a unilateral hemispinal injury, affecting the ipsilateral motor and dorsal column function and contralateral pain and temperature sensation; motor recovery occurs in 90%.
Spinal shock is caused by a depolarization of axonal membranes due to the kinetic energy imparted by trauma to the cord. All cord function distal to the injury is disrupted, including spinal reflexes. This can mimic complete cord injury and last for up to 24 hours. Resolution is marked by return of spinal reflexes (especially bulbocavernosus), at which time the extent of cord injury can be evaluated. This is to be differentiated from neurogenic shock, where loss of sympathetic outflow due to cord injury causes hypotension with bradycardia, normal urine output, and warm extremities. Treatment is by administration of peripheral vasoconstrictors.
Radiographs –
Radiographic evaluation of the cervical spine begins with the trauma lateral. This view should provide visualization of the occiput to T1. If soft tissue or the shoulders obscure the T1 superior endplate, then a swimmers view or a CT scan is necessary to evaluate the cervical spine. The lateral radiograph should be evaluated for smooth curves along the longitudinal lines of the anterior and posterior vertebral bodies, the lamina, and the spinous processes. The anterior soft tissues are evaluated for swelling, possibly representing a soft tissue injury of the spine. The width of the prevertebral soft tissues should be 6mm at C2 and 22mm at C6. The AP and odontoid (open mouth) views should be obtained if cervical spinal injury is suspected. Evaluation of the thoracic and lumbar spine should be guided by physical examination. Areas with tenderness to palpation or with neurologic changes (or in patients unable to participate in a physical exam) should be imaged with AP and lateral views. CT scan is a valuable adjunct in evaluating bony injury, and MRI is helpful in evaluating cord injury, nerve root compression, and soft tissue injury.
Treatment –
Although the specifics of treatment vary by the specific fracture pattern, certain guidelines are useful for all spinal injuries. If cord injury is suspected based on initial examination consideration should be given to instituting systemic steroid treatment. Based on the NASCIS trials, methylprednisone should be administered to minimize ongoing damage to the spinal cord with an initial bolus of 30mg/kg then at a rate of 5.4mg/kg/hr. If intiated within three hours of the injury the steroids should be given for 24 hours. If initiated 3-8 hours after the injury treatment should continue for 48 hours. After 8 hours, administration of steroids is not effective.
Initial management of spinal injuries begins with immobilization in the field with a backboard and rigid cervical collar or sandbags. Later treatment is aimed at achieving reduction and more effective immobilization. In the cervical spine reduction may be achieved through cervical traction with Gardner-Wells tongs (2 pins placed 1cm above the pinnae of the ears in line with the external auditory meatus bilaterally) or halo traction (4 pins at a pressure of 8 inch-pounds, anterior pins 1cm superior to the lateral 2/3 of the eyebrow, placed to avoid the supraorbital and supratrochlear nerves). Relative immobilization may be achieved with a rigid cervical orthosis or halo vest (eliminates 40% and 75% of atlantoaxial motion, respectively). More effective reduction and immobilization may be achieved with open reduction and fusion.
Achieving reduction of displaced, subluxated, or dislocated segments within the T&L spine is difficult to do closed and frequently requires open reduction. Relative immobilization may be achieved with a variety of braces, and operative fusion provides additional stability.
A. Cervical Spine Fractures and Dislocations
C1 Fractures –
The C1 ring has no vertebral body, instead articulating with the dens of C2. This articulation is stabilized by the transverse, cruciform, and alar ligaments. The transverse ligament, stretching between the lateral masses of C1 is the primary stabilizer. Evaluation of the C1 ring is best done on the dens (open mouth view). The interval between the dens and the lateral masses should be symmetrical (within 2mm) and there should be no overhang of the lateral masses of C1 on C2. On the lateral, the dens-basion interval should be measured at less than 10mm and the anterior axis-dens interval (ADI) should be less than 3mm. Increase in these distances or asymmetry suggests bony disruption of the C1 ring or ligamentous instability of C1-C2.
There are three basic types of C1 ring injury. Posterior arch fractures occur with a hyperextension mechanism and may commonly be associated with a fracture of the dens. Lateral mass fractures occur with an axial loading and bending mechanism. Burst or Jefferson fractures occur with axial loading and represent anterior and posterior arch disruption.
If nondisplaced, C1 ring fractures may be treated in a rigid cervical orthosis for 8-12 weeks. Displaced fractures, defined as greater than 7mm of lateral overhang of the lateral masses of C1 on C2, are treated with reduction by halo traction for 3-6 weeks followed by halo-vest immobilization. After treatment, flexion-extension views are obtained to look for persistent instability secondary to ligament disruption. An ADI 3-5mm represents injury to the transverse ligaments with the alar ligaments intact, while an ADI >5mm represents rupture of both the transverse and the alar ligaments. While traumatic C1-C2 instability may be treated with halo-vest immobilization initially, persistent instability requires C1-C2 fusion. C1-C2 fusion is also indicated in irreducible fractures or in cases where nonoperative treatment is not tolerated.
Atlantoaxial Rotatory Instability –
Atlantoaxial rotatory instability represents varying degrees of subluxation or dislocation of the lateral maases of C1 on C2 due to distraction and rotational forces. On the dens view, asymmetry of the C1 lateral masses with unilateral facet joint narrowing or overlap (wink sign) is suggestive of this injury. The lateral will demonstrate facet joint widening or subluxation/dislocation.
Treatment of traumatic atlantoaxial rotatory instability is traction reduction followed by halo traction for 4-6 weeks.
C2 Fractures –
Fractures of the odontoid process or dens of C2 are a common cervical spine fracture. Classification of these fractures is by location within the dens. Type I fractures represent avulsion injuries of the tip of the dens by the alar ligament, and may be treated with a rigid cervical orthosis until symptoms resolve. This fracture may rarely be associated with atlantoocciputal dissociation. Type II fractures are fractures at the base of the dens. This area is problematic as it is a watershed area that is bathed in synovial fluid and difficult to immobilize. Non-unions occur in up to 31% of Type II fractures treated non-operatively. Initial treatment should include closed reduction and halo immobilization. Operative treatment, consisting of C1-C2 posterior fusion or screw fixation of the dens, should be considered early in patients over 60 years old and in fractures displaced greater than 5mm, and late treatment in those that proceed to non-union. Type III fractures occur through the C2 body caudal to the base of the dens and can generally be effectively treated with halo immobilization.
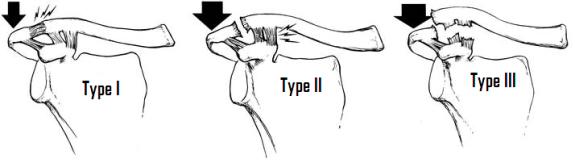
Hangman’s fractures are C2 posterior element fractures associated with C2-C3 traumatic spondylolisthesis. Type I are axial loading injuries resulting in a stable fracture of the neural arch through the pedicles with less than 3mm displacement. These fractures may be treated for 8-12 weeks in a rigid cervical orthosis. Type II fractures are caused by an axial loading and flexion injury displaced fractures of the pars intraarticularis. A subset of these fractures, type IIa, have injury to the discoligamentous complex as well, causing them to hinge on the anterior longitudinal ligament and angulate with traction. Type II fractures require a closed reduction followed by 12 weeks of halo vest immobilization. Type III fractures have bilateral pars intraarticularis fractures with dislocation of the facet joints. These injuries are extremely unstable and frequently associated with neurologic injury and usually require operative stabilization through fusion.
Lower Cervical Spine Injuries –
Cervical spine fractures below the C2 level are classified into 6 groups based on the mechanism of injury. Compression-flexion, or teardrop, injuries demonstrate varying degrees of anterior compression with widening of the posterior elements in more severe injuries. Vertical compression, or burst fractures, represent circumferential failure of the vertebral body with varying degree of displacement and canal compromise. Distraction-flexion injuries demonstrate widening of the posterior elements indicative of posterior ligamentous injury, and with severe injury unilateral or bilateral facet dislocation, or “jumped facet,” may occur. Compression-extension injuries result is unilateral or bilateral arch fractures with anterior subluxation of the injured vertebra on the vertebra below. Distraction-extension injury results in disruption of the anterior ligamentous complex or failure through the vertebral body with progressive failure of the posterior ligamentous complex and anterior subluxation. Lateral flexion injuries result in unilateral compression of the vertebral body. A special injury, the Clay-shoveler’s fracture, is an avulsion fracture of the C7 spinous process.
Stable injuries with minimal displacement and no neurological compromise may be treated non-operatively with a rigid cervical orthosis or halo vest for 8-12 weeks. Displaced fractures and facet dislocations are reduced using halo traction or Gardner-Wells tongs with gradual increase in weight and serial radiographs until reduction is achieved. Pre-reduction MRI of facet dislocation is frequently recommended to decrease risk of disk herniation and compression of the cord following reduction. Open reduction with decompression and stabilization is used in those fractures that fail closed reduction or have a neurologic deficit. Surgical approach is generally from the side of compression and stabilization involves fusion of one or more spinal levels.
B. Thoracic and Lumbar Spine Fractures
The Denis three column model of the thoracolumbar spine is critical to the evaluation of spinal fractures. In this model the spine is divided into an anterior column, including the anterior longitudinal ligament (ALL) and the anterior two-thirds of the vertebral body and disk, the middle column, including the posterior one-third of the vertebral body and disk and the posterior longitudinal ligament (PLL), and the posterior column, containing the neural arch, the ligamentum flavum, and the interspinous and supraspinous ligaments. Spinal stability is compromised with injury to two of the three columns.
From this model, fractures were further subdivided into one of four fracture types: compression fractures, in which the anterior column fails in compression and varying degree of kyphosis results; burst fractures, in which compression injury of the anterior and middle columns causes circumferential failure of the vertebral body with retropulsion of fragments into the canal; seat-belt injuries, resulting from flexion with the center of rotation anterior to the vertebral body causing failure of the anterior, middle, and posterior columns in tension (also known as a bony or ligamentous Chance fracture); and the fracture dislocations in which all three columns fail under one of three mechanisms, resulting in translation of the vertebra and canal compromise.
Treatment of thoracolumbar compression fractures is non-operative, and is directed at relieving symptoms. In the upper and middle thoracic spine, bracing may not be needed. In the lower thoracic and lumbar spine, a thoracolumbosacral orthosis (TLSO), corset, or Jewitt brace may be employed for comfort, as facture healing takes place over 8-12 weeks. In burst fractures, traditional guidelines for operative treatment included degree of canal compromise (>80%), kyphosis (>20˚), and anterior loss of height (>50%). Although still employed, these factors have become less important in surgical decision-making, and neurologic compromise has become the single most important indication for operative treatment. Non-operative treatment for burst fractures includes extended bed rest on a rotating bed, and brace treatment with a custom molded TLSO for fractures T7 and below or cervicothoracolumbosacral orthosis (CTLSO) for fractures above T7. Operative treatment should be employed for decompression of the fracture in the setting of a neurologic deficit and for stabilization when the fracture cannot be stabilized with bracing. Operative treatment consists of anterior or posterior fusion. Seat-belt injuries may be treated non-operatively with a custom molded TLSO, although injuries that are primarily ligamentous often do not heal well with non-operative treatment and may require operative stabilization with spinal fusion. Fracture dislocations are generally very unstable and associated with neurologic deficit, and operative treatment for reduction and stabilization is indicated.
C. Sacral Fractures
As the junction between the spine and the pelvis, sacral injuries may be discussed with either spinal fractures or pelvic ring injury. Sacral fractures are generally divided into three zones based on the Denis classification of sacral fractures: Zone I – alar fracture lateral to the neuroforamina; Zone II – transforaminal; Zone III – any fracture extending into the spinal canal. These fractures may compromise the lower lumbar and sacral nerve roots, and careful neurovascular and rectal examination should be documented.
Treatment is directed at ensuring lumbosacral and pelvic ring stability and preventing or relieving neurologic insult to the lumbosacral nerve roots. Non-operative treatment with restricted weight bearing or skeletal traction may be used. Operative stabilization may be performed with ORIF or percutaneous screw insertion. Finally posterior or anterior decompression and fusion may be indicated with neurologic compromise.