Osteosarcoma describes a sarcomatous lesion with characteristic bony elements. There are at least 9 different types of osteosarcoma. In this chapter we will discuss only the following: classic/intramedullary, periosteal, parosteal, secondary, and telangectatic.
Classic or high-grade intramedullary osteosarcoma is the most common and predominately affects males in 2nd and 3rd decade. It involves the metaphyseal region of bone and is usually located about the knee (50%) and proximal humerus. The hindfoot can also be affected. Symptoms of osteosarcoma often include pain that precedes any palpable mass, and an overlying nevus that expands is not uncommonly found. Ten to twenty percent of patients will have pulmonary metastases on presentation and as many as 90% will have micrometastases. The p53 gene has been implicated in the formation of osteosarcoma.
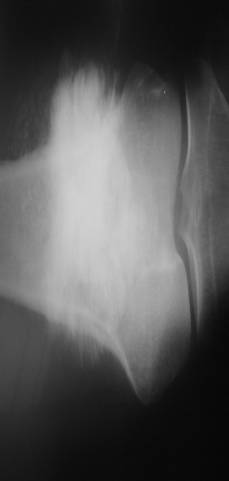
Radiographic appearance shows a permeative, lytic lesion of metaphyseal bone and the classic “codman’s triangle” is formed as the tumor pushes thru the cortex and raises the periosteum (Figure #14). The body then fills this void with bone creating a triangular structure. As many as 25% of presentations can have “skip lesions” or disease further along the bone than the original presenting lesion. Histologically, the unifying factor includes the presence of osteoid in a bed of pleiomorphic spindle cells that appear frankly malignant. A MRI should be obtained to delineate the borders of the lesion and involvement of surrounding structures such as neurovascular bundles and muscle.
Figure #14
Osteosarcoma of the distal femoral metaphysis.
www.sarcoma.org
Treatment of these lesions with simple amputation is historically grim with a survival of 10-20% long-term. This invariably was due to the presence of untreated micrometastases, and the picture has changed with the introduction of chemotherapeutic agents. Current regimens achieve 60-70% long-term survival and include pre-resection multiagent chemotherapy termed “adjuvant” chemotherapy (currently includes methotrexate, doxorubicin and ifosfamide) followed by re-staging, resection, and follow-up chemotherapy for 6-12 months. Following pre-resection chemotherapy, thebest prognosticator is tumor necrosis. Fifty percent of lesions will show rates of necrosis over 90%, which are associated with 85% 5-year survival.
Secondary osteosarcoma can arise within the setting of multiple conditions that include: Paget’s Disease, osteoblastoma, fibrous dysplasia, giant cell tumor, bone infarct, and chronic osteomyelitis. Patients tend to be older or elderly and the lesions involve the proximal humerus followed by the pelvis and femur. Classically, this disease presents with the new onset of pain overlying the usual dull achy pain associated with the primary disease (i.e. Paget’s). The new pain signals the presence of a new lytic lesion. The 5-year survival for this disease is 8% and most patients are too old to successfully tolerate chemotherapy.
Periosteal osteosarcoma is a low-intermediate grade variant that affects primarily the diaphysis of long bones and accounts for only 2% of osteosarcomas. It strikes mostly women in the 2nddecade of life. While the diaphyseal location means limb and joint salvage are often possible there is a high rate of metastasis and 25% will die in the first two to three years. The lesion forms just under the periosteum on the cortical surface and lifts the periosteum causing vigorous neo-osteogenesis. On plain film radiographs, this lesion is described as a sunburst-like lesion with a saucerized cortical depression. It has been likened to a “meteorite impact” with a lytic crater and a large amount of surrounding bone emulating impact debris. The differential includes aneurysmal bone cyst (ABC) and periosteal chondroma. Adjuvant chemotherapy, wide resection and maintenance chemotherapy are mainstays of treatment and this variant carries a slightly better prognosis than classic osteosarcoma.
Parosteal Osteosarcoma represents a low-grade variant that predominates in women. The lesions present mostly on the posterior aspect of the distal femur at the metaphyseal segment of bone and do not involve the medullary cavity (Figure #15).
Figure # 15
parosteal osteosarcoma of the distal femur.
www.sarcoma.org
Symptoms are generally absent other than a painless mass. Radiographs show a lobulated, ossified mass that appears “stuck on” to the cortex. Histologically these lesions show spindle cells with well-developed trabeculae and osteoblasts. Treatment includes wide surgical resection and small lesions can simply be removed with a single cortex. XRT and chemotherapy do not have a role unlessdedifferentiation has occurred within the lesion (found about one sixth of the time). Five-year survival rates are above 85% though lesions need to be followed for at least 10 years following resection as recurrence and dedifferentiation to high-grade sarcoma is possible and carries a poor prognosis.
Telangectatic Osteosarcoma, also known as hemorrhagic osteosarcoma, represents a high-grade variant that strikes in the second to third decade. This aggressive lesion has the same distribution as classic osteosarcoma, but advances rapidly and puts the patient at significant risk for pathologic fracture. Radiographically, this lesion is lytic and highly destructive. It has the same appearance as an aneurysmal bone cyst (ABC) and the two are easily confused. Histologically, the lesion appears as a hemorrhagic pool of blood with highly malignant appearing stromal cells interspersed. Treatment and prognosis are similar to high-grade osteosarcoma. However, the presence of pathologic fracture precludes limb salvage and pushes limb amputation into the forefront as the procedure of choice. Therefore, new lesions need strict protection while undergoing adjuvant chemotherapy.