Defined as difference in rate of growth between two limbs:
– usually due to abnormal physeal growth
– fracture malunions
– bone loss from osteomyelitis or tumor resections
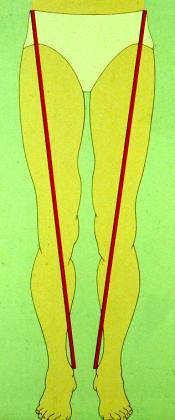
Evaluation includes determination of whether shortening is true or apparent.
Apparent limb length discrepancy (LLD) may be due to:
– suprapelvic obliquity
o scoliosis
– intrapelvic obliquity
o pelvic fracture
– infrapelvic obliquity
o hip contracture
o knee contracture
o ankle contracture
True Shortening Apparent Shortening
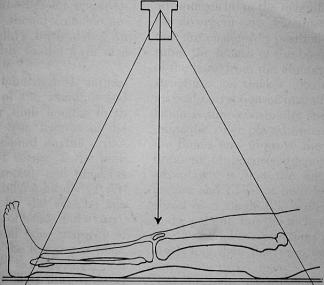
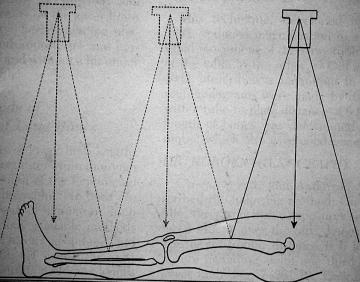
Assessment of true shortening involves measuring the absolute length of the limbs involving one of a number of methods:
– tape measure
– leveling the pelvis with blocks
– scanogram
– CT scans
– Long leg standing films
Why does leg length inequality matter?
– back pain
– scoliosis
– hip and/or knee osteoarthritis
A study by Gross (1978) showed & recommended:
– less than 2.0 cm showed no difficulties
– more than 3.5 cm, 80% had complaints
– LLD of 3 cm was compatible with high level sports
– Observation for less than 2 cm at maturity, especially if the patient has weakness or spasticity on the short side
Many options exist for limb lengthening, although are somewhat controversial:
– skeletally immature
o stapling
o epiphysiodesis
– skeletally mature for discrepancy greater than 3 cm
o lengthening using frame or IMN
o acute shortening, can fairly easily accommodate 8 cm in femur or 3 cm in tibia
– suggested approaches, given a normal height range are as follows:
o 0 – 2 cm: no treatment
o 2 – 6 cm: chow lift, epiphysiodesis, shortening
o 4 – 15 cm: lengthening procedure
o > 15 cm: prosthetic fitting
Epiphysiodesis
– first described by Phemiser in 1933
– performed by excising a square of bone from the medial and/or lateral margin of the growth plate and rotating it 90°
– permanent, difficult to undo physeal bar created if not satisfied with result
complications include miscalculation of timing and technical errors
Epiphyseal Stapling
– described by Blount in 1949
– potentially the same problems as the epiphysiodesis
– staples may be removed and physis will usually resume growth
The goal is equal limb length at maturity, unfortunately it is often difficult to predict future growth in a child. Stapling may permit less precise estimations whereas epiphysiodesis is unforgiving. Growth rates have been extensively studied and growth tables exist to help predict the growth remaining in a given limb at a given age. Growth is fairly constant from chronologic ages 6 to 9 with the femur growing roughly 2.0 cm (SD 0.27 cm) and the tibia 1.6 cm (SD 0.23 cm). During the adolescent growth spurt, yearly increments are extremely variable. Using bone age, rather than chronological age is a more useful and reliable gauge in predicting growth. This can be performed using standardized books containing figures of radiographs of the hand and wrist and comparing them to the patient. (Greulich)
Acute Shortening Procedures
– generally considered for patients with same amounts of LLD as those for epiphysiodesis but who are too old for correction with physeal closure
– femoral shortening usually preferred to tibial shortening
– up to 5 cm usually well tolerated in femur (3 cm in tibia), greater resulting in ineffective recovery of muscle-tendon units
– involves open shortening with plate fixation, proximal shortening with blade plate or newer closed femoral shortening using intramedullary nail
Growth Stimulation
– multiple techniques for stimulation of the short extremity have been tried with irreproducible and clinically insignificant results
o electrical stimulation
o sympathectomy
o surgical creation of AV fistulae
o placement of foreign bodies next to the physes
o packing bone beneath periosteum near physes
Limb Lengthening
– lengthening is generally reserved for patients with the most severe deformities
o multiple potential complications
- pin tract infections
- joint contractures
- joint subluxation or dislocation
- nonunion/malunion
o prolonged treatment times
– usually 4 to 20 cm
– relatively stable joints above and below are a prerequisite
– rotational or angular malalignment usually decreases total length attainable
– patient should be emotionally mature (usually older than 8 or 9 years)
– ring fixators have focused interest on the biology of lengthening
o rate of lengthening is critical
o osteogenesis begins in IM canal as multipotential cells diffentiate into osteoblasts
o bone formation resembles intramembranous growth (vs endochondral) as no cartilage matrix is laid down
o cells appear to lay down in longitudinal direction of retreating bone end
o patients allowed to fully weight bear and to do regular exercise to prevent joint contractures
– many modifications on the original theme (Ilizarov)
o uniplanar frame lengthening over an IM rod is becoming popular
– difficult decision concerning timing of removal of frame
Prosthetic Fitting
– generally least desirable form of treatment, but may be best choice with large discrepancy or severe deformity
– considered when predicted discrepancy at maturity exceeds 15 to 20 cm
– single operation vs multiple procedures and complications
– Syme amputation follows by prosthetic fitting results in a functional BKA that results in near-normal gait and activity level
o best performed when child is younger than 1 year
– for patient with severe proximal focal femoral deficiency, Syme with or without a knee fusion may be the best option
o Van Nes rotationplasty, which reverses the ankle joint to power a modified below-knee prosthesis is also an option (best if completed before 3 to 4 years)
Fortunately, growth disturbances are often not purely random and unpredictable. They are usually a progressive inequality due to growth in one extremity being inhibited. Studies have shown that 95% of patients with LLD have constant inhibition that is predictable over time. Polio is one example where the growth is usually not predictable.
Three common methods of predicting the future difference in LLD have been described:
– White and Menelaus (arithmetic method)
o Distal femur grows 0.9 cm/yr
o Proximal tibia grows 0.6 cm/yr
o Inaccurate in young children
o Uses chronological age, not skeletal
o Until maturity (15 ¼ for a girl and 17 ¼ for a male)
o Simplistic, but a good guide for timing of epiphysiodesis
– Green and Anderson (growth-remaining method)
o 100 kids from Boston (50% with polio) had their normal leg evaluated
o correlated growth to skeletal maturity with Greulich and Pyle bone age atlas
o accuracy improved by plotting over 3-4 yrs to assess growth inhibition
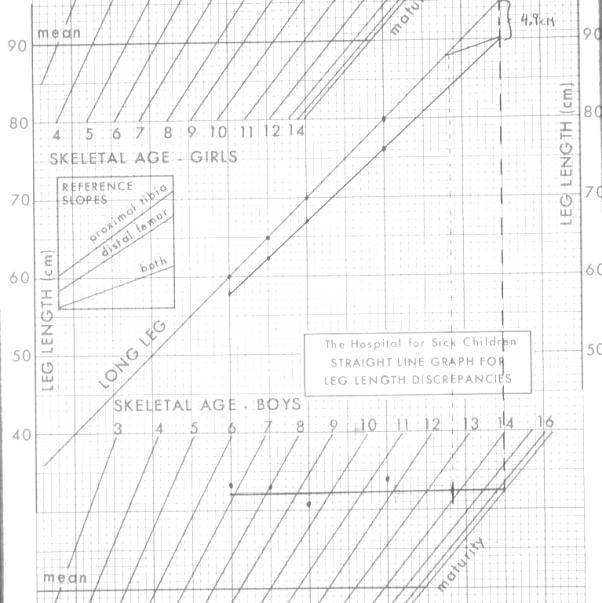
– Moseley (straight-line graph method)
o Derived from Green and Anderson data/tables
o Use more complicated straight line tables
In evaluating the various techniques used to assess limb-length discrepancy, studies vary with respect to interpretation of success. General success has been reported with both of these methods, although a recent review has reported rather disappointing results with all three commonly used methods, suggesting further refinement is needed.
| Determining Leg Length Discrepancy:The Arithmetic Method | |
| Leg Length Data(same data for all three samples)
Sex: Female
Age (yr) Skeletal age (yr) Right leg length (cm) Left leg length (cm) 7 + 10 8 + 10 66.0 58.2 8 + 4 9 + 4 64.4 61.9 9 + 3 10 + 3 70.0 66.2
|
|
| Prerequisite growth information
Distal femoral plate grows 10 mm/yr. Girls stop growing at 14 years of age. Proximal tibial plate grows 6 mm/yr. Boys stop growing at 16 years of age.
|
|
Assessment of past growth
= age at last visit – age at first
= 14 (16 for boys) – age at last visit
= present length – first measured length
|
= 9 yr 3 mo – 7 yr 10 mo = 1 yr 5 mo = 1.42 yr
= 14 yr – 9 yr 3 mo = 4 yr 9 mo = 4.75 yr
Long leg = 70 – 60 = 10.0 cm Short leg = 66.2 – 58.2 = 8.0 cm
= 7.04 cm/yr
= 0.2 cm |
Prediction of future growth
= years remaining X growth rate
= future growth of long leg X inhibition
= present discrepancy + future increase
|
= 4.75 X 7.04 = 33.4 cm
= 33.4 X 0.2 = 6.7 cm
= (70.0 – 66.2) + 6.7 = 10.5 cm |
| Prediction of effect of surgeryEffect of epiphysiodesis
= growth rate X years remaining |
Effect of epiphysiodesis Femoral = 0.9 X 4.75 = 4.28 cm Tibial = 0.6 X 4.75 = 2.85 cm Both = 1.6 X 4.75 = 7.13 cm
|
Taken from Chapman’s Volume 4, p. 4347.
| Determining Leg Length Discrepancy:The Growth Remaining Method | |
| Prerequisite growth information
Distal femoral plate grows 10 mm/yr. Girls stop growing at 14 years of age. Proximal tibial plate grows 6 mm/yr. Boys stop growing at 16 years of age.
|
|
Assessment of past growth
= present length – first length
= length of long leg – length of short leg
|
= 70.0 – 60.0 = 10.0 cm
= 66.2 – 58.2 = 8.0 cm
= 70.0 – 66.2 = 3.8 cm
= 0.2 |
Prediction of future growth
= mature length – present length
= future growth long X inhibition
= present discrepancy + future increase |
= 81.1 – 70.0 = 11.1 cm
= 3.8 + 2.2 = 6.0 cm
|
Prediction of effect of surgery
|
= 2.7 cm
Correction from distal femoral arrest = 4.1 cm
Correction from combined arrest = 2.7 + 4.1 = 6.8 cm
|
Taken from Chapman’s Volume 4, p. 4348.
Moseley Straight-line Graph Method
Generously donated by James Roach, M.D.
Most images and much of the general information from this section were “borrowed” from a powerpoint presentation by James Roach, M.D. Much was also “borrowed” from Chapman’s, Volume 4, Chapter 170 ‘Limb-Length Discrepancy in Children’.