A. Pelvic Ring Fractures
Pelvic ring fractures represent one of the few true life-threatening emergencies in orthopaedics. Prompt recognition of unstable pelvic ring injuries and appropriate treatment are critical to preserving life and preventing significant disability.
Anatomy –
The bony pelvis is composed of the two innominate bones joined anteriorly in the midline by the pubic symphysis and posteriorly through strong ligamentous attachments to the sacrum. The innominate bones are formed by the fusion of the ilium, the ischium, and the pubis at the triradiate cartilage at skeletal maturity. The anatomy of the pelvis is such that the weight of the body is transmitted from the vertebral column to the sacrum, though the sacroiliac joints and the strong sacral ligaments to the innominate bones, and into the lower extremities through the weight bearing surface of the acetabulum.
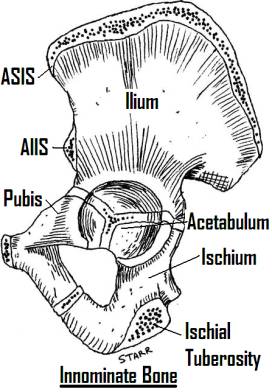
The pelvis is often described as a ring structure, although perhaps it is better described as a cylinder enclosing the abdominal and pelvic viscera. The false pelvis lies above the pelvic brim, is enclosed by the iliac wings, and contains the abdominal viscera. The pelvic brim, or inlet, is marked by the arcuate line, which runs along the superior pubic rami anteriorly, along the ilium to join the ala of the sacrum and sacral promontory. Below this line lies the true pelvis, which contains the pelvic viscera. Distally, the pelvic outlet is bordered by the inferior pubic rami, the ischium, and the sacrotuberous ligaments to the distal sacrum and coccyx.
The ligamentous anatomy of the pelvis is critical to its stability. Anteriorly, a fibrocartilagenous disc connects the pubis bones at the symphysis. Posteriorly, the sacroiliac joints, stabilized by the anterior and posterior (ventral and dorsal) sacroiliac ligaments and the interosseous ligaments, and the sacrotuberous and sacrospinous ligaments are important in maintaining the stability of the pelvic ring.
Vascular injury in the pelvis may be life-threatening, and a thorough understanding of vascular anatomy of the pelvis is critical. The median sacral artery is unpaired and derives from the aorta at its bifurcation. The aorta bifurctates into the common iliac arteries at L4, further dividing into the internal and external iliac arteries at the sacral ala. The external iliac arteries travel along the medial border of the psoas at the pectineal line, giving off the inferior epigastric artery and the deep iliac circumflex arteries before passing under the inguinal ligament in the femoral canal as the femoral arteries. The internal iliacs branch into anterior and posterior components at the S1 level. The anterior component becomes the internal pudendal artery to the external genetalia, the inferior gluteal artery, and the obturator artery. The posterior component supplies the superior gluteal artery, as well as the iliolumbar and lateral sacral arteries. The obturator artery runs on the sidewall of the pelvis to exit the pelvis through the obturator foramen, and may give off a branch that anastamoses on the posterior surface of the pubis with the inferior epigastric artery or external iliac. This anastamosis is called the corona mortis, and may be at risk when dissecting the posterior surface of the pubis.
The venous anatomy of the pelvis mirrors the arterial anatomy. The inferior vena cava branches slightly more distally than the aorta (L4-5), and equivalent venous branches accompany the arterial branches through the pelvis.
The lumbosacral plexus of nerves supplies the lower limbs, receiving contributions from T12-S3. The lumbar plexus lies above the pelvic brim along the lumbar spine, and may be divided into the dorsal branches, which supply the ilioinguinal (T12-L1), iliohypogastric (T12-L1), genitofemoral (L1-2), femoral (L2-4), and lateral femoral cutaneous (L2-3) nerves, and the ventral branches, which supply the obturator nerve (L2-4). The sacral plexus lies in the true pelvis on the anterior surface of the piriformis, and may also be divided into a dorsal division which supplies the superior (L4-S1) and inferior (L5-S2) gluteal nerves and the common peroneal portion of the sciatic nerve, and a ventral division, which gives rise to the tibial portion of the sciatic nerve (L4-S3) and pudendal nerve (S2-S4).
Pelvic ring injuries are generally high-energy fractures, frequently seen in MVAs, motorcycle accidents, falls from heights, auto-pedestrian accidents, and activities such as bull and horseback riding. The history of the exact mechanism of injury, including the type and magnitude of force, direction of force, and position of the patient on impact is critical to understanding the character of the injury, and has major implications as to the classification, treatment and prognosis, as discussed below.
As a high-energy injury, pelvic fractures are frequently associated with other injuries. Examination of the patient should begin with a trauma evaluation, beginning with the ABCs to assess hemodynamic status and primary survey. Secondary survey should include assessment of pelvic stability in the AP and vertical planes by stressing the pelvis. This should be done only once, by the most senior examiner, as repeat examinations of an unstable pelvis may exacerbate vascular injury by dislodging clots. The method for assessing pelvic stability includes gentle pressure over the anterior superior iliac spine.
Secondary survey should include examination of the rectum for gross blood and position of prostate, vagina and perineum for tears, contusion or Morel-Lavallée lesion (cutaneous-fascial separation), and urethral meatus for blood. A full musculoskeletal examination should be performed to look for other injuries.
Insufficiency fractures in elderly patients should be considered separately from high-energy pelvic ring disruptions. The mechanism is generally low-energy (ground-level fall, saddle injury after falling in bathtub). These injuries generally do not require a trauma work-up, and the stability of the pelvic ring is rarely compromised. Typically, the injury is an anterior isolated pubic ramus (superior and/or inferior) fracture (although subtle posterior injury may occur).
Radiographic examination of pelvic ring injuries frequently begins with the trauma AP pelvis. Inlet and outlet plain film views should be obtained early, as they are critical to the classification of the fracture and the evaluation of potential instability and the need for operative stabilization or traction. CT scan may be a useful adjunct if obtained for other reasons (ie. pelvic injury, hemorrhage), but is of less value than the plain films for most pelvic ring injuries.
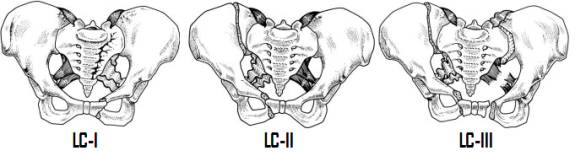
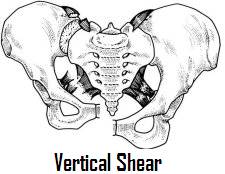
The Young classification of pelvic ring injuries is most often used. It describes the injury based on the direction of the force on the pelvis (lateral compression (LC), anteroposterior compression (APC), vertical shear (VS), and combined) and subdivides these groups (LC and APC) into I-III based on degree of destabilization of the pelvic ring.
In lateral compression fractures the force is directed from the side (as in a side-impact MVA) causing the side of impact to collapse inward. Classification is based on the radiographic appearance of the inlet view. Anteriorly, unilateral or bilateral superior and inferior pubic rami fractures with or without symphysis injury is observed. Posteriorly, the amount of disruption seen determines the degree of stability. As the lateral force is directed inwards, the sacrotuberous and sacrospinous ligaments are shortened rather than stressed and are rarely disrupted; therefore, these fracture are not typically associated with increased pelvic volume. LC-I fractures typically demonstrate a buckling of the sacrum through Zone II (or less frequently Zone I). This buckle fracture is typically relatively stable (at least initially). LC-II fractures have a characteristic vertical fracture of the posterior iliac wing, which may or may not extend into the SI joint. As the ligaments are intact, these fractures are relatively stable, although they may be vertically unstable with weight bearing due to the acetabulum being detached from the axial skeleton both anteriorly and posteriorly. LC-III fractures are windswept deformities of the pelvis, typically seen when an individual is run over by a car – LC-II injury on the side of initial contact along with a secondary external rotation injury to the contralateral side, disrupting the sacrotuberous, sacrospinous, and anterior sacroiliac ligaments. The side of secondary impact typically demonstrates AP instability and neurologic injury from stretch of the lumbosacral plexus.
Anteroposterior compression injuries result from an impact directly on the pubis or bilateral ASIS or ischial tuberosities, resulting in an external rotation force or “open-book” injury. These injuries may be seen in motorcycle injuries or auto-pedestrian impacts from directly in front. Again, the stability of these fractures is determined by the integrity of the ligaments posteriorly. Classification is again based on the appearance of the inlet view. Anteriorly, the pubic symphysis is widened to an increasing degree with increasing grade. In APC-I injuries, the symphysis is widened less than 2cm, and a slight widening of the anterior SI joint which may not be readily apparent. These fractures are stable to AP and vertical stress. APC-II injuries demonstrate a pubic diastasis, along with opening of the anterior SI joint secondary to incompetence of the anterior SI ligaments as well as the sacrotuberous and sacrospinous ligaments, resulting in severe AP instability with increase in pelvic volume. APC-III injuries demonstrate disruption of anterior and posterior SI ligaments in addition to the sacrotuberous and sacrospinous ligaments, resulting in a profoundly unstable pelvis in both the AP and vertical planes with increase in pelvic volume. This pattern is associated with high rates of neurologic and vascular injury and with hemorrhage.
Vertical shear injuries occur when the pelvis is stressed longitudinally, as occurs with a fall from height onto a straight lower extremity or MVA. Best seen on an outlet view, the hemipelvis will be displaced cephalad, and like the APC-III injury, this pattern represents disruption of all of the posterior ligaments, resulting in a vertically unstable pelvis.
Initial treatment of pelvis ring fractures should be focused on treating hemodynamic instability. Providing adequate volume of blood products and fluids in the initial resuscitation period to maintain perfusion is critical. If the pelvic volume is increased (open-book pelvis), reducing pelvic volume and sheeting the patient with a bed sheet spread 6 inches and centered over the greater trochanters will effectively decrease this volume and reduce the space available for hemorrhage. Taping the patient’s toes together will help to resist the external rotational force seen in open book pelvis fractures. Continued hemodynamic instability should lead one to suspect arterial injury, treated by angiography with arterial embolization.
Once hemodynamically stable, assessment of the fracture may begin. Vertically unstable fractures should be placed in skeletal traction (either femoral or tibial) with 10-20% of body weight, with traction films to confirm reduction. Stabilization of a sheeted unstable pelvis fractures should ideally be undertaken within 24 hours to prevent skin necrosis.
Stable fractures may be treated closed. Insufficiency fractures may be treated with progressive weight bearing as tolerated. LC-I and APC-I fractures may be treated non-operatively with restricted weight bearing on the side with the posterior ring injury, but frequent radiographic evaluation is necessary to ensure that these injuries do not secondarily become unstable.
External fixation is effective at providing anterior stabilization and closing down pelvic volume in APC-II fractures, but provides little stability for fractures that are grossly unstable posteriorly and may require adjunctive posterior stabilization. It is useful when time is a consideration, or when there is concern for contamination, as in an open injury or an injury associated with bowel or bladder injury.
ORIF of the pubic symphysis and pubic rami may be undertaken to provide anterior stabilization. Posterior stabilization with SI plating or percuaneous SI screws effectively treats posterior instability.
Extremely high incidence of DVT (49-61%), pelvic thrombosis (29-35%), symptomatic pulmonary embolus (2-12%), and fatal thromboembolism (0.5-10%) make thromboembolic disease the most dreaded complication of pelvic fractures. Mechanical and chemical prophylaxis should be instituted as soon as is deemed safe, and permanent or removable vena cava filters used as adjuncts when effective anticoagulation is not possible.
B. Acetabulum Fractures
Acetabular fractures are a difficult group of fractures to treat, as experience has shown that only anatomic reduction of the weight-bearing surface of the hip joint will provide satisfactory results. Even in the most experienced hands, this anatomic reduction is achieved in only 70-74% (Letournel and Judet). Recognition of operative fractures and appropriate initial treatment are essential to give the patient the best chance of a good result.
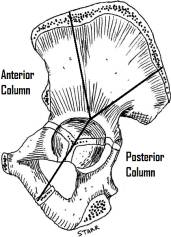
The acetabulum is formed at the confluence of the ilium, ischium, and pubis. A hemispherical horseshoe-shaped articular surface is supported by two columns of bone arranged as an inverted Y. The anterior column is composed of the iliac crest, the iliac spines, the anterior wall and anterior one-half of the acetabulum, and the superior pubic ramus and is represented radiographically by the iliopectineal line. The posterior column is composed of the dense bone superior to the sciatic notch, the posterior wall and posterior one-half of the acetabulum, and the ischium and ischial spine, and is represented radiographically by the ilioischial line. The dome or roof of the acetabulum is the weight-bearing surface that supports the femoral head. The quadrilateral plate lies medial to the acetabulum and is the thin flat plate of bone that forms the lateral wall of the true pelvis.
As acetabular fractures are frequently associated with high-energy mechanisms such as MVA, trauma evaluation is often necessary. Pain may be present with range of motion of the hip. If the hip is dislocated, the position of the leg may offer a clue as to the direction of dislocation – internally rotated for posterior, externally rotated for anterior. A careful neurovascular exam to determine function of the sciatic nerve, femoral nerve, and lateral femoral cutaneous nerve should be documented as nerve injury may be present in 30% of acetabular fractures.
Radiographic evaluation of an acetabular fracture requires an AP radiograph as well as Judet views (45º iliac and obturator obliques). The iliac oblique will allow evaluation of the posterior column and anterior wall, while the obturator oblique allows evaluation of the anterior column and posterior wall. A CT scan should be obtained for evaluation of the degree of displacement, comminution, and marginal impaction of the fracture, as well as to ensure concentric reduction of the hip.
The classification system of Letournel and Judet is the most commonly used. It divides acetabular fractures into simple and associated types.
Initial treatment of an acetabular fracture revolves around achieving a concentric reduction of the hip. Large fractures of the posterior wall, dome, or medial wall of the acetabulum may be associated with instability or frank dislocation. Reduction of the dislocation is urgent, as markedly poorer results are associated with persistent dislocation of over twelve hours. Once the fracture has been evaluated radiographically for stability and the anatomy of the dislocation is well understood, one to two attempts at closed reduction with sedation in the emergency room may be attempted. Failing this, closed reduction with general anaesthesia and paralysis may be attempted. An irreducible dislocation is an indication for emergent open reduction and internal fixation. If a fracture is reducible but unstable, skeletal traction may be implemented to hold the reduction.
Non-operative treatment of acetabular fractures is appropriate for fractures with concentric reduction of the femoral head without instability that do not involve the weight-bearing dome or posterior wall of the acetabulum. In addition, patient factors such as ambulatory demand and ability to tolerate surgery must be taken into account. Weight bearing as tolerated is the primary mode of non-operative treatment. Skeletal traction may be used for treatment of nondisplaced weight-bearing dome fractures or in fractures associated with instability of the hip if the patient cannot tolerate ORIF.
ORIF should be considered for patients who demonstrate instability out of traction, have a fracture involving the weight-bearing dome (as defined by a roof-arc angle of less than 45º on any of the AP or Judet views or fracture line within 1cm of the top of the dome on CT), or have a posterior wall fracture greater than 40% on CT. Surgery should be done within a week of injury. A variety of approaches may be used depending on the anatomy of the fracture, the most common being the iliofemoral (and extended iliofemoral), ilioinguinal, Kocher-Langenbach and triradiate. A variety of implants, including lag screws, pelvic reconstruction plates, and spring plates may be used for fixation.
Patients with acetabular fractures are at a high risk for venous thromboembolism. Mechanical and chemical prophylaxis should be initiated as soon as prudent after admission and continued postoperatively. IVC filters should be used if chemical prophylaxis is not a valid option. Following surgery, prophylaxis against heterotopic ossification is prudent as HO occurrence ranges from 9-62% following operative treatment. Patients should be non-weight bearing for 6-8 weeks following ORIF of the acetabulum.

