LCPD is an osteonecrosis of the femoral head that occurs because of unknown reasons STEPHANIE. This apparent idiopathic osteonecrosis has been associated with second hand smoke, older parental ages, low normal patient stature and protein C&S deficiencies. There is however no known definitive causes. It can, although rarely, run in families.
Presentation:
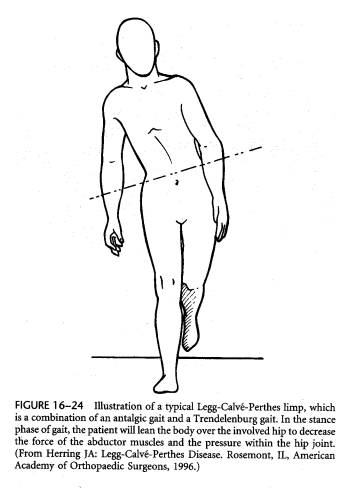
Perthes occurs generally between 3-9 years of age and occurs boys to girls 5:1. The difference in incidence due to gender may be secondary to the fact that boys have an incomplete intracapsular ring of proximal femoral vessels more often than girls. Perthes may be bilateral in 10% of cases, although the two sides do not occur simultaneously and therefore will be at different stages of disease. Children usually present with a Trendelenburg or antalgic gait with limitation of abduction and inward rotation.
The pain may present in the anterior thigh and/or knee region delaying diagnosis as knee pathology is pursued. In pediatrics, thigh/knee pain is hip pathology and should be studied with an AP pelvis and through hip exam. Occasional severe synovitis can occur, and fluctuation of pain intensity is common. Nearly 90% of children have a delay in bone age compared with chronologic age.
Imaging:
An early standing AP pelvis can have very subtle findings such as slightly increased radiodensity or shortening of height in the femoral head.
A frog lateral may be positive first, with a small subchondral fracture noted. Once the diagnosis is established both a standing AP pelvis and abduction internal rotation (AIR) view are used to help with staging and treatment.
Classification:
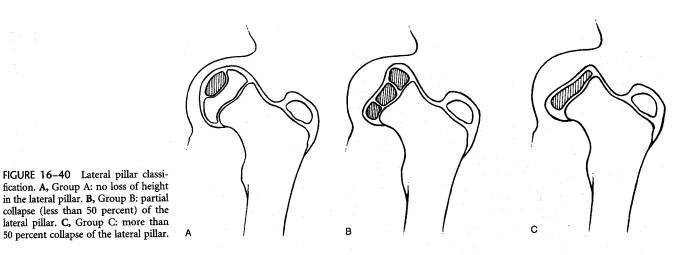
Historically the Catterall and Salter/Thompson classification schemes were used; presently the Herring classification is most commonly employed since it has excellent inter/intra observer reliability, is easy to use and has prognostic implications. The Herring classification judges the “lateral pillar” of the femoral head on standing AP pelvis (lateral 1/3 of the femoral head). In Group A there is no decrease in height, In Group B more than 50% of height is maintained, and in Group C less than 50% of height of the lateral pillar remains.
Natural History
The natural history of Perthes disease is that the hip will regenerate blood supply and repair itself with time (often a two or more year process). The hip progresses (as described by Waldenstein) frominitial phase (around six months) to fragmentation stage (around eight months) to reossification stage (20-50 months) to resolved stage. The resolved hip shows stigmata of disease such as coxa breva (short femoral neck), coxa magna (large femoral head), ovoid femoral head shape, and at worst a femoral head that does not match the acetabulum. Incongruence of this type leads to early osteoarthritis (i.e., 3-4th decade).
Treatment focuses on maintaining the femoral head within the acetabulum and also congruence of the femoral/ acetabular relationship.
Prognostic Factors:
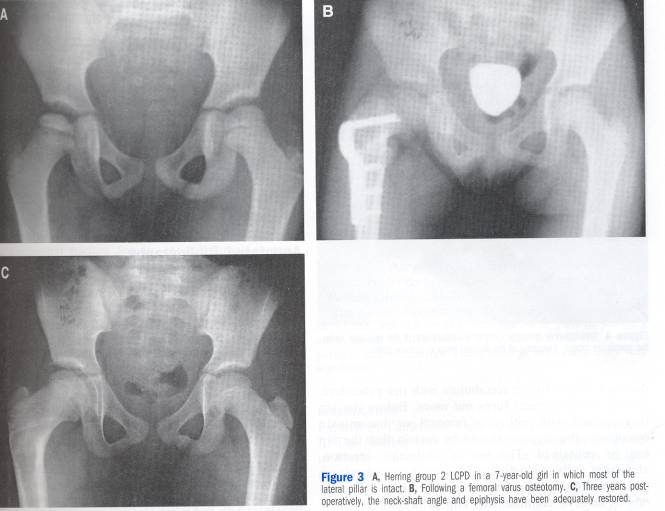
There are multiple “head at risk” signs seen on plain AP pelvis radiographs. These are lateral calcifications to the femoral head, femoral head extrusion out of the acetabulum >20%, a horizontal physis, metaphyseal cysts, or a wide femoral neck. Most important is Herring stage and age at onset of the disease. Herring A hips do well regardless of age and Herring C hips do poorly, (although in children <5 years they still may have an adequate outcome). In Group B Herring hips, children older than eight have a guarded prognosis, and children less than eight years must be carefully watched. Group B children older than eight do best with early femoral osteotomy.
Treatment:
The principles of treatment are to:
1. Maintain motion (both to add fluid to the joint and minimize epiphyseal flattening).
2. To avoid lateral extrusion (buzz words are “maintain containment”) of the femoral head.
The child is evaluated at 2-3 month intervals during the fragmentation stages to assess motion and containment of the femoral head (seen on AP pelvis). Activity modification is often suggested to minimize loading impact on the fragile femoral head. Stretching and low impact activities such as swimming, karate and biking are suggested. If the pelvis film shows extrusion of the femoral head lateral to Perkins line, an AIR pelvis film (abduction internal rotation) is taken to assess how the position of the femoral head would be improved if the femoral head were “tucked in” to the acetabulum. The AIR therefore mimics what would occur if a varus osteotomy of the femur is done. Varus osteotomies with or without soft tissue releases of the adductor, iliopsoas and/or medial capsule are the mainstays of surgical treatment of Herring B and C hips.
Some centers have used a Salter osteotomy (pelvic) for treatment, but multicenter studies suggest this may not be as effective as a varus femoral osteotomy. Doing osteotomies of the hip after fragmentation stage will not change the shape of the femoral head significantly at skeletal maturity and are not indicated except for salvage. The use of hip abduction braces (Texas Scottish Rite brace, etc.) has not been found to change the natural history of the disease.
Outcome
Children must be followed well into the resolved phase of the disease. Serious later sequelae such as hinge abduction or joint incongruity lead to early osteoarthritis. Poor outcomes are more likely in the older child, or one with collapse and extrusion of the lateral femoral head (Herring C). Hips with these problems can have a valgus osteotomy to put the round portion of the head in the acetabulum or if necessary a total hip arthroplasty.
In hips where coax breva (short neck) occur due to involvement of the proximal femoral physis, the greater trochanter can be relatively too cephalad making the hip abductors (which insert on the trochanter) biomechanically disadvantaged and leading to a Trendelenburg limp.
A valgus osteotomy or trochanteric transfer can improve this problem but not often completely reverse it.
The Stulberg classification of long term outcome is used in many studies to define post Perthes hip health after skeletal maturity. Group I has normal appearance, II has loss of head height, but good congruence with a “ mostly round” head, in group III the head is elliptical, but the acetabulum matches the deformity(congruous incongruity). In group IV the head and acetabulum are flat and in group V the head is flat and the acetabulum is round leading to joint incongruity. Group I and II have good prognoses while group III has a guarded prognosis. Groups IV and V will develop osteoarthritis by their forties, often necessitating early arthroplasty.
Conclusion
Perthes disease is an ailment of young children ages 3-9, often male, which affects the blood supply of femoral head. Although self limited, serious consequences to the growth and architecture of the proximal femur can occur, especially in children over the age of 8 at disease onset. Careful and frequent evaluation of both clinical exam and radiographs is required during the active phase of the disease. Surgery is often required for the older child, or one with advanced disease.