A. Distal Femur Fractures
A distal femur fracture is variably defined as a fracture of the femur 9-15 cm proximal to the articular surface of the femoral condyles. These fractures may be supracondylar or intracondylar. Distal femur fractures are relatively rare (7% of all femur fractures), and occur in a bimodal distribution with a peak in young, active males, which represents a high-energy fracture associated with significant trauma, and a second peak in the elderly, which generally represents a lower-energy mechanism, such as a ground-level fall.
On presentation, these limb may demonstrate shortening, apex-posterior angulation, crepitus, and tense swelling of the knee. A thorough neurovascular exam is critical due to the proximity of the tethered popliteal artery. Vascular injury occurs in 2-3% of distal femur fractures, increasing to 40% with concomitant dislocation of the knee. Open injuries occur in 5-10%, usually anterior, proximal to the patella. Associated injuries to the femur, knee ligaments (in 20%), and tibial plateau or shaft are not uncommon.
Anatomy –
The distal femur flares at the diaphyseal-metaphyseal junction to form two condyles, covered in articular cartilage. Anteriorly, there is a depression for the articulation of the patella. Posteriorly, the condyles are separated by a deep intercondylar fossa. The articular surface of the lateral condyle is broader and flatter than the medial condyle, while the medial condyle is more convex and extends farther distally, to give the knee 7-11º of physiologic valgus. The femoral shaft is aligned over the anterior half of the condyles.
Muscular attachments of the distal femur include the adductor magnus on the adductor tubercle medially, and the gastocnemius posteriorly at the articular margins of the medial and lateral condyles. The quadriceps anteriorly and the hamstrings posterior-medially may also be deforming forces.
The popliteal artery is tethered in this location, proximally as it passes through the adductor hiatus 10 cm from the joint, and distally at the soleus arch.
Radiographs and Classification –
AP and lateral radiographs of the femur, knee, and hip are necessary for initial examination. Traction views may be helpful in comminuted or widely displaced fractures, as well as 45° oblique films to assess intracondylar fracture. CT scans, MRI, or angiography may rarely be used in initial evaluation.
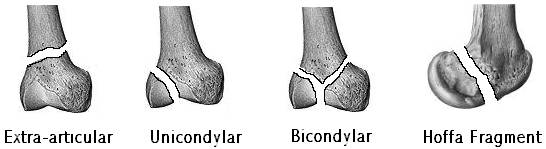
The OTA classification system separates these fractures into three general types: extra-articular (type A), partial articular or unicondylar (type B), and complete articular or bicondylar (type C). These categories are further subdivided based on complicating factors. However, clinically, these fractures are usually simply described based on location (supracondylar/intracondylar), pattern (transverse, oblique, spiral), displacement, angulation, comminution, and special fracture patterns, such as a coronal split of the condyle (Hoffa fragment).
Treatment –
Closed treatment of distal femur fractures may be considered in several instances: when operative treatment is contra-indicated by medical condition, when the patient is a non-ambulator, when the bone quality is too poor to accept fixation, or when the fracture is too severely comminuted to repair. Immobilization or traction may be used in these instances. In addition, non-displaced or stable fractures may be treated by immobilization and restricted weight-bearing.
ORIF is the standard of care for unstable or displaced fractures. This includes anatomic reduction of the articular surface using lag screws, followed by fixation of the distal femur to the shaft using intramedullary devices, fixed angle devices (95º blade plate, dynamic condylar screw, or locking condylar plate), or buttress plates.
External fixation is used primarily as a temporizing measure when soft-tissue or patient instability precludes definitive fixation.
B. Knee Dislocations and Patella Fractures
i. Knee Dislocation
Knee dislocations are a rare entity, accounting for less than 1.2% of orthopedic trauma. Many of these injuries go unrecognized, however, as the knee may spontaneously reduce in 20-50%, and the significant morbidity associated with these injuries make prompt recognition crucial.
The mechanism of injury may be low- or high-energy. Low-energy injuries are usually sports-related and result from hyperextension with varying degrees of varus or valgus stress, resulting in anterior dislocation. High-energy injuries are frequently seen in MVAs and may result from hyperextension or dashboard injury, with the knee flexed 90º and force directed posterior.
Anatomy –
Frequently damaged structures in knee dislocations include the ligamentous stabilizers of the knee and the popliteal artery and vein. The anterior and posterior cruciate ligaments originate from the lateral and medial condyles of the femur respectively and insert onto the tibia near the tibial spine in the intertubercular sulcus, providing stability in anterior and posterior translation of the tibia on the femur as well as some rotatory stability. The medial and lateral collateral ligaments originate from the femoral epicondyles and insert on the proximal tibia and proximal fibula respectively, providing resistance to varus and valgus stresses. Secondary stabilizers, such as the posterior-lateral capsular structures, may also be compromised.
The popliteal artery is particularly susceptible to injury in dislocations due to its tethering proximally at the adductor hiatus 10 cm proximal to the knee and distally at the soleus arch. Popliteal artery injury has been reported in 8-64% of dislocations and has been shown in cadaver studies to occur at 50º hyperextension.
Classification –
Two types of classification systems exist for knee dislocations – directional and anatomic. Directional describes the dislocation by the direction of the tibia in relation to the femur:
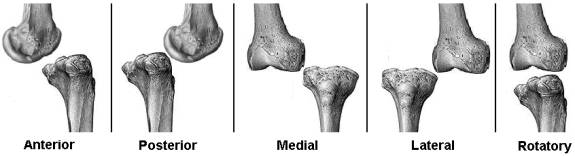
The anatomic classification describes the ligamentous, vascular, and nervous structures compromised in the injury:
- KD I = either ACL or PCL torn (collaterals usually torn);
- KD II = both ACL and PCL torn, collaterals intact;
- KDIII = ACL/PCL torn, one collateral torn, designated by L or M
- KDIV = ACL/PCL/MCL/LCL and posterior-lateral corner torn.
- Designators C and N denote vascular (C) or neural (N) injury.
Evaluation and Treatment –
Immediate reduction of the dislocation is necessary to relieve occlusion of arteries, tension on nerves, and pressure on skin. This may usually be accomplished closed, although open reduction may occasionally be indicated. Evaluation of the injury should include a thorough neurovascular exam pre- and post-reduction (peroneal nerve injury in 14-35%, vascular injury in 8-64%), and plain radiographs to look for associated fractures. Arteriography, arterial Doppler ultrasound, and MR angiography may have a role to evaluate vascular injury (versus serial examinations in the presence of normal pulses). Finally, MRI to evaluate ligamentous damage may be considered early.
Non-operative treatment by immobilization of the knee in slight flexion for 6 weeks may be considered, but results are generally not as good as operative treatment. Most recommend early operative ligamentous repair either as a one-stage operation or as a two stage (PCL/LCL/PLC early, ACL late) operation.
i. Patella Fractures
Patella fractures account for approximately 1% of all fractures. They are of two basic types: high-energy fractures resulting from a fall onto a flexed knee, resulting in a complex stellate fracture pattern, or low-energy fractures resulting from sudden forceful contraction of the extensor mechanism overcoming the tensile strength of the patella, resulting in a simple or transverse fracture patterns. They are seen most commonly between ages 20 and 50, and occur in men twice as often as in women.
Physical Exam –
Patella fractures will often present as a painful hemarthrosis, with or without soft-tissue compromise. The hemarthrosis may be aspirated, followed by injection of sterile saline (if concern for an open joint exists) or lidocaine for analgesia. After injection of lidocaine, a straight leg raise will test for patency of the extensor mechanism.
Radiographs –
Basic radiographs should include AP, lateral, and sunrise views. On the AP view, the fracture pattern may often be most easily seen. Evaluation of the position of the patella on the AP should reveal a patella in the midline of the femoral sulcus and with its distal pole within 2 cm of a line drawn perpendicular to the femoral condyles. On the lateral view, position of the patella should be evaluated , as a high-riding patella (patella alta) or a low-riding patella (patella baja) may be indicative of patellar tendon or quadriceps tendon rupture, respectively. Insall’s ratio, or the ratio of the greatest diagonal length of the patella to the patellar tendon length judged on the lateral radiograph should be 1 +/- 0.2. In addition, the superior pole of the patella should lie below a line extending from the anterior cortex of the femur with the knee flexed to 90º.
Classification –
Classification of patellar fractures is generally by fracture pattern and degree of displacement. Non-displaced patellar fractures are generally associated with an intact extensor mechanism and can frequently be treated non-operatively. Displaced fractures may have an intact extensor mechanism, but will frequently require operative intervention. Common fracture patterns are shown below.
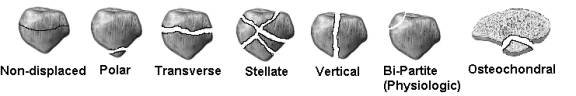
Failure of fusion of a growth plate in the patella may result in a bipartite patella, an anatomic variant occurring in 8% of individuals and frequently confused with fracture. A bipartite patella will be an irregularly-shaped fragment with smooth edges in the superior-lateral corner of the patella. It will be bilateral in the majority of cases.
Anatomy –
The patella is a sesamoid bone, suspended between the quadriceps tendon proximally and the patellar tendon distally. It is invested in a fascial structure formed by the coalition of the quad tendon, the iliotibial band, and the fascia lata, which form the medial and lateral retinacula, which may account for an intact extensor mechanism in the presence of a complete, displaced fracture of the patella. The blood supply to the patella is from a dorsal anastamotic ring supplied by the geniculate vessels, entering the patella primarily through the middle of the anterior body of the patella and retrograde from the distal pole vessels. The patella is susceptible to avascular necrosis following fracture.
Treatment –
Treatment of patellar fractures may be non-operative for non-displaced fractures with an intact extensor mechanism. This involves immobilization in a cylinder cast, knee immobilizer, or hinged knee brace locked in extension.
Operative treatment of patellar fractures usually includes the techniques of lag screw fixation, tension banding, cerclage wiring, and partial or complete patellectomy used in combination depending on the fracture pattern.
C. Tibial Plateau Fractures
Injuries to the proximal weight-bearing surface of the tibia, or tibial plateau, account for 1% of all fractures, but 8% of fractures in the elderly. They occur in a bimodal distribution, with high energy fractures occurring in the young secondary to falls from heights, car bumper injuries, and strong valgus or varus forces as occur in football games or skiing, and a second peak in the elderly from low energy, relatively minor valgus forces causing lateral injuries. 55-70% of tibial plateau injuries are lateral injuries, with higher energy medial (10-20%) and bicondylar (10-30%) fractures accounting for the rest.
History and Physical Exam –
A careful history of the mechanism leading to a tibial plateau fracture will allow classification of the fractures as high or low energy, giving some indication to the amount of soft tissue compromise associated with the injury. On exam, a tense, swollen knee will be seen, as the injury is intraarticular. A thorough neurovascular exam should be conducted to rule out popliteal artery injury and peroneal or tibial nerve injury. Varus and valgus testing should not be done, as this may displace a previously non-displaced fracture.
Examination of the condition of the soft tissues is critical. Open wounds should be examined carefully to determine communication with the joint or an open fracture. This determination may require injection of the joint with sterile saline to test for fluid extravasation. The presence and degree of contusion and swelling (as shown by the presence of skin wrinkles) should be noted. Fracture blisters, representing seperation of the epidermis from the underlying dermis should be noted as clear versus hemorrhagic (denoting a deeper dermal injury which may not be safe to incise). Compartment syndrome of the leg should likewise be evaluated.
Radiographs and Classification –
Initial radiographs should include AP and lateral views of the knee. 40° internal and external oblique films may be useful in further evaluating the fracture. CT scan is a useful adjunct for pre-operative planning to examine for the presence and degree of articular depression. Some advocate the use of MRI to evaluate for meniscal or ligamentous damage, but it is unclear that this alters the immediate surgical plan in the majority of cases.
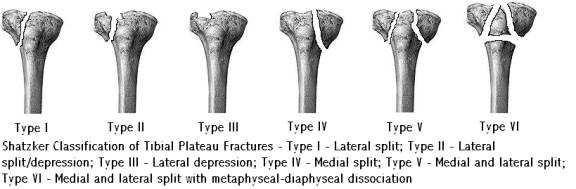
The most common classification system for plateau fractures is the Shatzker Classification. It is simple, descriptive, and separates to some extent low (Types I-III) from high energy (Types IV-VI) fractures.
Anatomy –
The proximal tibia is divided into medial and lateral tibial condyles, separated by the intercondylar eminence, composed of the medial and lateral tibial spines and the areas for insertion of the cruciate ligaments and menisci. The proximal tibia has a slope of 10° from anterior to posterior and is perpendicular to the long axis of the tibia in the coronal plane. The menisci sit atop the medial and lateral plateaus.
The medial plateau is the larger of the two, and is concave in both the sagittal and coronal planes. The cartilage of the medial plateau averages 3mm thick, and the subchondral bone is stronger and more resistant to fracture than the lateral plateau.
The lateral plateau is smaller and more proximal (important in evaluation of the lateral radiograph) than the medial plateau. It is convex in both the coronal and sagittal planes and the cartilage is slightly thicker (4mm).
Treatment –
Many factors must be taken into account to determine the correct treatment for a tibial plateau fracture and the timing of that treatment. Fracture characteristics such as the location, pattern, amount of displacement and degree of joint incongruity can be evaluated radiographically. Just as important, however, are factors such as joint stability, soft tissue compromise (including open fractures, shear injuries, edema and fracture blisters, as well as neurologic and vascular injury), and patient factors, such as associated injury, medical stability, age, bone stock, and pre-injury activity level.
Articular incongruity of less than 3mm (some authors will allow for incongruity as much as 1cm) is well tolerated in the tibial plateau without significantly affecting long-term outcome. Critical to preserving knee function is early range of motion to prevent arthrofibrosis and a stiff knee.
Closed treatment may be considered in closed fractures that are non- or minimally displaced, or when patient factors preclude operative treatment. Low energy fractures (elderly with lateral plateau fx) respond better to closed treatment than do high energy fractures. Both fracture and joint stability must be evaluated prior to closed treatment. Closed treatment should allow for protection from varus and valgus stresses as well as early range of motion. This may often be accomplished in a hinged knee brace. The patient should be non-weight bearing.
Traction may rarely be used in multiply-injured or unstable patients with significant comminution. This should be combined with early range of motion.
Operative treatment by ORIF is the treatment of choice for most tibial plateau fractures. Open, unstable, significantly displaced, or high energy fractures should be considered for operative treatment. Timing of surgery is determined by the condition of the soft tissues, and surgery may be delayed 1-2 days to 1-2 weeks in high energy fractures. A joint-spanning external fixator may be a useful adjunct in cases where definitive fixation must be delayed.
ORIF of tibial plateau fractures may include simple lag-screw fixation in split type fractures, joint surface elevation and bone grafting in depressed fractures, buttress plating or fixed-angle plating or a combination of these techniques. Arthroscopy may have a role in evaluating reduction or elevation of the joint surface. External fixators with skinny-wire fixation may be used as definitive treatment (rarely) or as an adjunct to ORIF. Regardless of the type fixation, anatomic reduction with early range of motion is the goal of treatment.

