A. Talus
The talus is the second-most commonly fractured tarsal bone. The talus is very mobile, articulating within three joints that together account for 90% of the motion of the foot. This mobility makes the talus susceptible to injury and makes anatomic reduction of talus fractures critical to maintaining hindfoot function.
Anatomy –
The talus is composed of a body, neck and head, and posterior and lateral processes. The talar body is wedge-shaped, wider anteriorly than posteriorly and largely covered by articular cartilage. The talar neck extends from the body distally, deviating medially approximately 15-20º. The talar neck and head have relatively decreased bone density medially and inferiorly, making these areas susceptible to comminution. The posterior process of the talus extends from the talar body and is divided into medial and lateral tubercles by the flexor hallicis longus tendon. The lateral process extends from the talar body and articulates with the posterior facet of the calcaneus and the distal fibula.
The talus lies beneath the tibia within the mortise as part of the ankle joint, articulates with the calcaneus at the subtalar joint and with the navicular at the Chopart joint. These extensive articulations necessitate that 60% of the surface area of the talus be covered by articular cartilage. The talar neck is bare of articular cartilage, and is the site of insertion of the ligamentous and vascular insertions. The talus does not have any musculotendinous attachments.
The vascular supply to the talus is very tenuous, and like other areas where the blood supply is largely retrograde, the talus is susceptible to osteonecrosis following fracture. The blood supply is primarily from branches entering the undersurface of the talar neck from an anastamotic sling formed by the artery to the tarsal sinus laterally (from the dorsalis pedis and peroneal arteries) and the artery to the tarsal canal medially (from the posterior tibial artery). The artery to the tarsal canal gives off the deltoid branches which supply the medial third of the talar body, branches from the dorsalis pedis enter the neck dorsally, and capsular and ligamentous branches also have contributions.
Neck Fractures –
Talar neck fractures are generally high-energy injuries, and as such are associated with ipsilateral calcaneous fracture (10%), malleolar fracture (19-28%) and tibiofibular diastasis. Classically associated with rudder-box injures from WWI-era plane crashes, they are now more commonly seen with brake pedal injury in MVAs. The patient will present with pain, swelling, and distortion of the hindfoot, and open injury may be seen in 16-25%. Dislocation of the ankle, subtalar, or Chopart joint may be seen, often in the posterior-medial direction, and prompt reduction should be undertaken to lessen skin slough.
Radiographic evaluation includes AP, lateral, and mortise views, as well as a Canale view, which is taken with the ankle in maximal equines, the foot pronated 15º, and the X-ray beam angled 75º cephalad. This view provides maximum exposure of the talar neck.
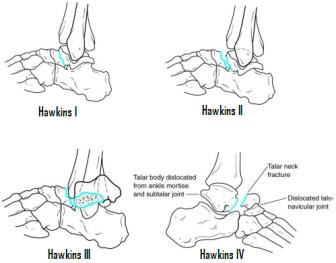
The Hawkins classification is commonly used to describe talar neck fracture-dislocations, classifying fractures I-IV based on degree of subluxation or dislocation of the talar body. Type I fractures are non-displaced fractures of the talar neck. Type II fractures are minimally displaced with subluxation or dislocation of the subtalar joint. Type III fractures are fractures with dislocation at the ankle and subtalar joints. Type IV fractures, added to Hawkins’ original classification are fractures with dislocation of the ankle, subtalar and talonavicular joints.
Treatment of talar neck fractures is based on the Hawkins grade. Type I fractures may be treated with a below-knee cast and non-weight-bearing for 8-12 weeks. Type II fractures may be treated with closed reduction and casting in slight equinus for 6 weeks and at neutral for 6 more weeks, for a total of three months non-weight-bearing, or may be treated with ORIF with one or two cannulated screws anterior to posterior or posterior to anterior up the talar neck. Type III and Type IV fractures should undergo a prompt reduction to avoid skin slough (which often requires open reduction), and irrigation and debridement if necessary. A medial malleolar osteotomy or a calcaneal traction pin may be necessary to achieve reduction of the talus. Compression screws AP or PA may be used for internal fixation, and delayed primary closure may be necessary at 5-7 days to avoid skin slough.
Complications frequently encountered after talar neck fracture include skin necrosis, infection, delayed/non-union, malunion, post-traumatic arthritis, and osteonecrosis (occurring in 0-13% of Type I, 20-50% of Type II, and 80-100% of Type III and IV fractures). Hawkins sign is the rarefication of the talar body seen after talar neck fracture, indicating resorption secondary to disuse osteopenia and when present is a sign of revascularization of the talar body. MRI may provide a more accurate evaluation of AVN when clinically suspected.
Talar Body Fractures –
Osteochondral fractures of the talar dome are frequently seen in young men after a twisting injury and may be associated with ankle fracture. They usually occur anterio-lateral and poterio-medial on the talar dome. The treatment of this injury is based on symptoms: symptomatic lesions require no treatment, symptomatic lesions require excision of small fragment and ORIF of larger fragments. Ankle arthroscopy with drilling of defects may also play a role in treatment.
Lateral process fractures, or “snowboarder’s ankle,” occur with dorsiflexion/inversion injuries and represent avulsion injuries of the lateral talocalcaneal ligament. This injury presents with tenderness at the tip of the lateral malleolus and may be confused with an ankle sprain. The fracture may be seen on AP and mortise radiographs. Non-displaced fractures should be treated with non-weight-bearing in a below-knee cast for six weeks. Single, large, displaced fragments may be closed reduced versus ORIF, and comminuted fractures may require excision of fragments.
Posterior process fractures may involve the lateral tubercle, the medial tubercle, or both. Lateral tubercle fractures may be inversion injuries resulting in avulsion by the posterior talofibular ligament, or may result from forced plantarflexion, in which the lateral tubercle is compressed between the calcaneus and tibia. Medial tubercle fractures may occur in pronation of a dorsiflexed foot, resulting in avulsion by the posterior fiber of the deltoid ligament. Lateral tubercle fractures should be treated initially in a below-knee cast and protected weight bearing for 4-6 weeks, and may require excision of the fragment. Medial tubercle fractures may be treated closed or may require ORIF as the fragment is often large and interposition of the flexor hallicus longus may block closed reduction.
Subtalar Dislocations –
Subtalar dislocation of the foot may occur with inversion (medial dislocation, 80-85%) or eversion (lateral dislocation, 15-20%). They may occur in falls from heights, MVAs, or as a sporting injury (esp. basketball). Subtalar dislocations are frequently associated with fractures, and are open injuries in 10-40%. Prompt reduction to prevent compromise of the skin tented over the talar head is critical. Closed reduction may be blocked by the tibialis posterior tendon in lateral dislocations and extensor digitorum brevis tendon or talonavicular capsule buttonholing with medial dislocations, requiring open reduction. Immobilization in a below-knee cast for four weeks following reduction allows the soft-tissues to heal.
B. Calcaneus
Calcaneal fractures remain a challenge to orthopaedists. The most commonly fractured of the tarsal bones, they are frequently seen in falls from heights and MVAs. The majority of calcaneal fractures are high-energy fractures that may be associated with injuries to the spine, contralateral calcaneus, or ipsilateral lower extremity in 50% of cases. These fractures cause massive swelling of the hindfoot, and a clinically detectable compartment syndrome may develop in 10%. The condition of the soft tissue and social factors such as smoking and worker’s compensation involvement may drastically affect the outcome of the treatment, and are critical in surgical decision-making.
Anatomy –
The calcaneus has been described as similar to an egg, with a hard cortical shell surrounding soft cancellous bone inside. The posterior half of the calcaneus is composed primarily of the tuberosity and is the site of the insertion of the Achilles tendon complex and the plantar fascia. The anterior half of the calcaneus is occupied dorsally by the posterior, middle, and anterior articular facets of the subtalar joint. Anteriorly it articulates with the cuboid bone. Medially, the sustentaculum tali projects from the body and supports the middle facet, with the flexor hallicus longus tendon passing under the sustentaculum tali. Laterally, an anterior process supports the anterior facet, a peroneal trochlea projects laterally above the groove for the peroneus longus tendon, and a lateral process of the tuberosity on which the plantar fascia originates.
Radiographs and Classification –
Radiographic evaluation of the calcaneus should begin with AP and lateral views of the hindfoot, as well as a Harris view, taken with the foot in maximum dorsiflexion and the X-ray tube angled to obtain a tangential view of the heel, which may delineate the amount of widening of the hindfoot, loss of height, and articular involvement. Broden’s view, which allows evaluation of the articular surface of the posterior facet, may be obtained by internally rotating the lower extremity 45º and directing the X-ray tube 10-40º cephalad. This is useful intraoperatively, although it has largely been replaced by CT scanning for pre-operative planning.
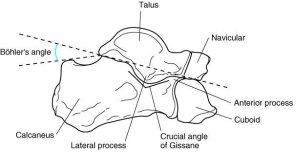
The lateral radiograph should be evaluated for loss of calcaneal height, as noted by a decrease in Böhler’s angle, which is described as the complement of the angle formed by a line from the highest portion of the anterior facet to the highest portion of the posterior facet and a second line from the highest portion of the posterior facet to the highest portion of the calcaneal tuberosity. This angle should normally measure 25-40º. The crucial angle of Gissane is the angle formed by the downward portion of the posterior facet where it connects to the upward portion. It should measure around 100º, and if increased may represent impaction and loss of height of the posterior facet.
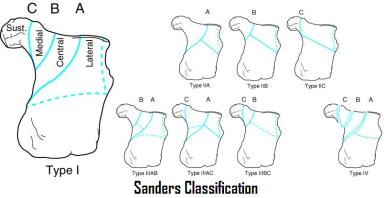
CT scans are now done routinely prior to surgical intervention. They provide accurate information regarding the intraarticular portion of the fractures. There are many different classification systems used, most based on CT images of the posterior facet. The Sanders classification is commonly used, and is based on the number (I-IV) and location (A-C) of fracture lines as seen on the coronal images of the posterior facet.
Treatment –
Treatment of calcaneal fractures is controversial. Initially, all fractures are treated with immobilization in a bulky Jones-type compressive dressing to limit swelling. One to two weeks may be needed for swelling to subside to the point that further treatment may be initiated.
Due to high rates of complications and variable results with operative treatment, many calcaneus fractures may be treated non-operatively, especially those with factors that are known to produce poor outcomes, such as smokers and worker’s compensation patients. Non-operative treatment consists of a short period of immobilization, followed by early range of motion and 6-8 weeks of non-weight-bearing. Closed manipulation with or without percutaneous pinning may also be considered.
For displaced intraarticular fractures or fractures that lead to unacceptable deformity, ORIF may be undertaken. This usually involves a lateral approach in which the fragments are fixed to the constant fragment of the sustentaculum tali. Primary subtalar fusion is an option for treatment in severely comminuted fractures.
For extraarticular fractures, such as anterior process, sustentaculum tali, or peroneal tubercle fractures, those with small fragments may be treated closed in a below-knee cast. Some may require excision of a comminuted or symptomatic fragment. Finally, those fractures with large fragments may be treated with ORIF by a single screw.
C. Lisfranc Injuries
Injuries to the tarsometatarsal joint, or Lisfranc joint, may present a diagnostic challenge to the treating orthopaedist, as often they reduce spontaneously and the resulting ligamentous instability may not be apparent on the initial radiographs. 20% may go unrecognized initially, leading to a course of prolonged pain and morbidity, and untreated Lisfranc injuries may cause significant disability long-term.
The Lisfranc joint complex plays a role in maintaining the two major arches of the foot, the transverse arch and the medial longitudinal arch. The Lisfranc ligament is a large ligament on the plantar surface of the foot which runs from the lateral corner of the medial cuneiform to the base of the second metatarsal, and helps to maintain these arches.
Two major mechanisms commonly lead to Lisfranc injuries – longitudinal loading of the foot in fixed equinus (as occurs in sports injuries and falls from heights) and crush injuries to the midfoot. On presentation, the patient will have pain in the foot with weight bearing and with passive range of motion of one or more metatarsal heads. The patient may also have point tenderness over the involved areas. Plantar ecchymosis in an area confined to the base of the first and second metatarsals is frequently associated with injury to the Lisfranc ligament, which may lead to collapse of the arches of the foot with weight bearing.
Initial radiographic evaluation should include weight-bearing AP, lateral and oblique views of the foot. Non-weight bearing views may show the joint in an anatomic alignment which may hide the instability associated with these injuries. Stressing these ligaments with weight bearing views will reveal this instability with lateral migration of the second metatarsal from its anatomic alignment with the medial border of the middle cuneiform or with widening of the interval between the first and second ray, especially between the medial cuneiform and base of the second metatarsal. Comparison views with the contralateral foot may be helpful. CT scan may play a role in evaluating these injuries for subtle fractures or soft tissue injury.
Early recognition and prompt treatment of these injuries is crucial to preventing collapse of the arch of the foot and long-term disability. Injuries that present with pain with weight bearing and point-tenderness but no instability (defined as a shift greater than 2mm from anatomic position) may be treated closed with a below-knee cast and a short period (~3 weeks) of non-weight bearing followed by progressive weight bearing as tolerated. Unstable injuries should undergo ORIF with stabilization of the compromised ligamentous structures, followed by 6-8 weeks of non-weight bearing.
D. Other fractures
Metatarsal Fractures –
Metatarsal fractures may occur with a crush injury to the foot or with a torque mechanism. They may be associated with swelling, pain with weight bearing, point tenderness, and ecchymosis. Injuries to other parts of the foot should be ruled out, such as a Lisfranc fracture or ligament rupture. Radiographic evaluation should include AP, lateral, and oblique views of the foot, weight bearing if possible.
First metatarsal fractures may require treatment because of the significant deforming forces that they face. One third of the weight seen by the forefoot is supported by the first metatarsal. The attachments of the peroneus longus and tibialis anterior on the first metatarsal base exert significant influence on the alignment of the metatarsal head and consequently the medial forefoot. If there is no evidence of instability on stress radiographs, these fractures may be treated with progressive weight bearing in a below-knee cast. Instability or deformity should be addressed with either closed reduction and percutaneous pinning or ORIF. Fusion of the tarsal-metatarsal or metatarsal-phalangeal joint may be necessary to restore stability in intraarticular fractures.
Fractures of the second, third, or fourth metatarsals usually exhibit stability due to the soft tissue interconnections between these bones. Dorsal-plantar deviation greater than 10º may result in transfer metatarsalgia and should be corrected surgically. Translation greater than 3-4mm should likewise be addressed. Otherwise, these fractures may be treated with weight bearing as tolerated in a hard soled shoe.
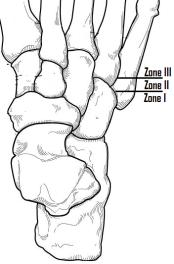
Fractures of the base of the fifth metatarsal may be further divided into three zones based on location of the fracture, as the mechanism of injury, treatment, and prognosis varies with anatomic location. Zone I injuries are typically avulsion fractures of the tubercle of the fifth metatarsal. They occur with inversion injuries, and represent avulsion of the attachment of the plantar aponeurosis (the peroneus brevis, which also inserts at this level, appears to have little effect on fracture pattern). These fractures are generally stable and may be treated symptomatically in a hard-soled shoe or walking boot, although symptoms may last for 6-8 weeks.
Zone II injuries are true Jones fractures, representing an adduction injury to the forefoot and fracture at the proximal metaphyseal-diaphyseal junction. These injuries typically heal well, as they possess a good metaphyseal blood supply, and may be treated in a below-knee cast with weight bearing as tolerated for 8-10 weeks.
Zone III injuries are diaphyseal fractures and frequently represent stress fractures. The proximal 1.5cm of the diaphysis of the fifth metatarsal is an area of increased stress and a watershed area between the metaphyseal and diaphyseal blood supply. Repetitive cyclic loading leads to chronic pain, followed by completion of the fracture. These fractures may be treated closed in a short leg cast and non-weight bearing for 2-3 months until symptoms resolve. The high rate of non-union seen with closed treatment of Zone III fractures may lead to ORIF with bone grafting and intramedullary fixation with a single screw.
Dancer’s fractures are fractures of the diaphysis of the fifth metatarsal. They may occur with rotational and axial loading of a plantar-flexed foot, or with rolling over the outer border of the foot. They may be treated closed with 8 weeks weight bearing as tolerated in a short leg cast.
Phalangeal fractures –
Fractures of the proximal phalanx are the most common phalangeal fractures of the foot. They may occur with a crush mechanism or an axial loading (stubbing the toe). These fractures are typically stable may be treated closed with treatment in a stiff-soled shoe. Closed reduction may be needed if clinical deformity is present, with attention paid to alignment and rotation. Persistent instability may require ORIF.