A. Hip Dislocations and Femoral Head Fracture
i. Hip Dislocations
Hip dislocations are an uncommon injury, usually associated with motor vehicle accidents (dashboard injuries) or other high energy mechanisms. They are associated with other fractures up to 50% of the time, including ipsilateral acetabular, femoral neck, and femoral head fractures.
Classification of hip dislocations is based on the direction of the dislocation and the associated fractures. Posterior dislocations account for 85-90% of dislocations, with anterior and obturator dislocations accounting for the remainder. Sciatic nerve injury may be observed in 10-20% of posterior dislocations.
Treatment of the dislocated hip is dependent on the associated injuries present. Expedient reduction of the hip decreases the risk of osteonecrosis of the femoral head; however, concomitant femoral neck fracture, acetabular fracture, or femoral head fracture may make a closed concentric reduction impossible or ill-advised. In these cases, open reduction with treatment of the associated injuries is indicated.
Prognosis varies widely in hip dislocations, with 70-80% good to excellent results with simple dislocations, decreasing rapidly with associated fractures and delayed relocation. Osteonecrosis (5-40%), post-traumatic arthritis, nerve injury (50-60% permanent), and heterotopic ossification formation complicate treatment.
ii. Femoral Head Fractures
Femoral head fractures are an uncommon entity, usually occurring in a high-energy trauma and associated with acetabular fractures, hip dislocations, and femoral neck fractures. They frequently occur as dashboard injuries, as a flexed hip is thrust backward and the head is fractured on the rim of the acetabulum. The Pipkin classification system is used to describe these injuries:
- Type I: Posterior dislocation of the hip with fracture of the femoral head caudad to the fovea centralis
- Type II: Posterior dislocation of the hip with fracture of the femoral head cephalad to the fovea centralis
- Type III: Type I and type II with associated fracture of the femoral neck
- Type IV: Type I, II, or III with associated fracture of the acetabulum

Treatment may include non-operative treatment, excision of the fragment, or ORIF depending on the size, location, and displacement of the fragment as well as the associated injuries.
B. Hip Fractures
Epidemiology –
Hip fractures are a common entity associated with significant morbidity and mortality, and resulting in a significant financial burden to society. There were 280,000 hip fractures in the US in 1998, and $8.7 billion was spent to treat these injuries. This represents 43% of the money spent on fracture care in the US. To the individual, a hip fracture corresponds to a significant threat to life and independence, with a 13-37% mortality rate at one year and decreased ambulatory ability and chance of returning to an independent living situation.
Risk fractures for hip fracture parallel those of all osteoporotic fractures: increasing age (the risk of fracture multiplies by 100 from age 65 to 85), female sex, Caucasian race, dementia, poor health, previous osteoporotic fracture, urban setting, tobacco use, low body weight, inactivity, alcohol use, sedatives, anti-hypertensives, corticosteroids and laxatives have all been associated with increased risk of femur fracture.
Hip fractures in young people are much more rare than in the elderly, and usually represent high energy injuries. The prognosis and treatment of these injuries is frequently quite different than in the elderly population.
History and Physical Exam –
Mechanism of injury leading to hip fractures in elderly patients is usually a ground level fall. Important aspects of the history include the reason for the fall, loss of consciousness before or after the fall, risk factors for fracture, co-morbidities, living situation, ambulatory status, and presence of pre-injury hip pain. These elements may give clues to underlying medical problems that may be addressed before surgery, as well as help determine the course of treatment and help determine prognosis. Overall, one can expect an elderly person with a hip fracture to lose one level of ambulation (independent, cane, walker, non-ambulatory).
On physical exam, the leg will classically be shortened and externally rotated if displaced. Careful examination for associated fractures (concurrent wrist fractures occur in 5-10% of hip fractures) and for sacral and heel decubitus ulcers is important. AP and cross-table lateral radiographs (with the contralateral hip flexed to 90) allow adequate imaging without manipulating the injured hip.
i. Femoral Neck Fractures
Anatomy –
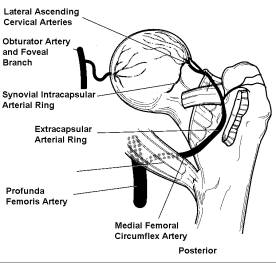
The anatomy of the femoral neck is of importance in understanding the particular difficulties encountered in treatment of this fracture. Lying within the capsule of the joint, the fracture line is bathed in synovial fluid. The high stresses seen within the hip joint and the angles of the fracture and femoral neck often dictate that the fracture line is under significant shear or even distraction forces, leading to non-union. Finally, the limited and unprotected blood supply to the femoral head is frequently interrupted, leading to avascular necrosis of the femoral head and collapse.
The cervical arteries are the primary blood supply to the femoral head. These arteries are fed by an extracapsular ring, which is in turn fed by contributions from the medial femoral circumflex posteriorly and the lateral femoral circumflex anteriorly. The cervical vessels pierce the capsule near its insertion on the neck and ascend parallel to he neck, reconstituting an intracapsular ring and enter the femoral head adjacent to its inferior articular surface. The superior/posterior vessels from the medial femoral circumflex are the larger and more numerous of the cervical vessels. In addition, 75% of hips have a significant contribution to femoral head from the foveal artery (a branch of the obturator artery).
Classification –
The most frequently used system to describe femoral neck fractures is the Garden classification. It essentially divides femoral neck fractures into stable, non-displaced fractures (Garden I and II) and unstable, displaced fractures (Garden III and IV).
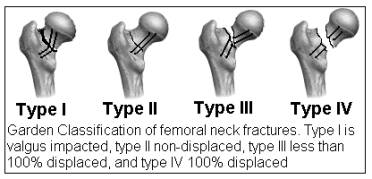
The Pauwells classification is based on the obliquity of the primary fracture line and is useful in evaluating the risk of non-union in neck fractures treated by ORIF. As Pauwell’s angle increases, forces seen by the fracture shift from compressive to shear and finally to distraction forces, leading to higher non-union and AVN.
Treatment –
Treatment of femoral neck fractures varies with the age of the patient and the displacement of the fracture, as well as with region. In older folks with low energy fractures, generally Garden I and II fractures are treated with closed in situ pinning with three cannulated partially threaded cancellous screws down the femoral neck. Garden III and IV fractures are generally treated with hemiarthroplasty vs total hip arthroplasty (in the setting of preexisting arthritis).
In young people, an attempt is usually made to save the femoral head and avoid arthroplasty. Therefore, Garden I and II fractures would be treated by in situ pinning while a Garden III or IV fracture would be treated by closed reduction and pinning vs ORIF.
Complications of treating femoral neck fractures include AVN (in 33% of displaced fractures), non-union, hardware cut-out or failure, and infection.
ii. Intertrochanteric and Basicervical Fractures
Intertrochanteric fractures are more closely associated with osteoporosis and co-morbidity than are femoral neck fractures. The patients who sustain these injuries tend to be sicker, and less ambulatory than those with other hip fractures.
Anatomy –
Intertrochanteric fractures have a much better prognosis for healing than femoral neck fractures due to anatomic considerations. The intertrochanteric region is extracapsular, so the fracture is not bathed in synovial fluid. Being metaphyseal, the intertrochanteric region is primarily dense trabecular bone, which provides both for stability from interdigitation and a healthy metaphyseal blood supply. The calcar femorale, a dense strut of trabecular bone from the posterior-medial shaft to the posterior femoral neck provides medial stability.
Classification –
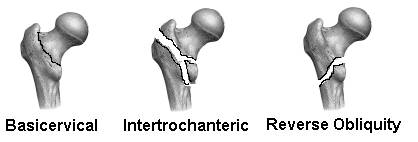
The most common classification systems used to describe intertrochanteric fractures are the Boyd and Griffin Classification, which describes four types based on the obliquity and displacement of the fracture, and the Evans Classification, which attempts to describe the stability of fractures based on the integrity of the posterior-medial cortex. However, these classifications are rarely used in practice, and a simple description of the level (basicervical, intertroch +/- subtroch extension), obliquity (reverse obliquity unstable due to pull of the adductors on distal fragment), and degree of medial comminution are used clinically to describe the fractures.
Treatment –
Non-operative treatment has limited applicability in intertrochanteric fractures, reserved only for the most medically unstable patients, or non-ambulators with minimal discomfort. Surgical stabilization is the standard of care for most intertrochanteric fractures. Most treatments allow impaction of the fracture edges, encouraging healing. This includes fixed angle sliding nail plate devices, such as the sliding hip screw or the Medoff plate, or cephalomedullary sliding hip screw devices such as the Gamma nail, which provide more biomechanical stability, critical in fractures with subtrochanteric extension or reverse obliquity patterns. Rarely, trochanteric replacing arthroplasty may be indicated in severely comminuted fractures.
iii. Subtrochanteric Fractures
Subtrochanteric fractures may be divided into low-energy (osteoporotic) fractures in the elderly, high-energy fractures in the young, and a significant number (17-35%) of pathologic fractures. The leg will be shortened, and may have varus angulation due to pull of abductors, flexors and external rotators on the proximal fragment and adductors on the distal fragment. In the high energy fracture, associated injuries should be evaluated (5-6% incidence of ipsilateral femoral neck fractures, 30% undetected).
Classification –
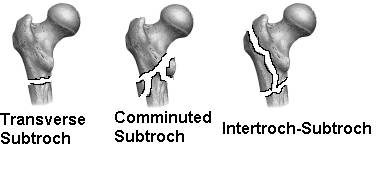
No one classification system has proven itself to be clinically superior to the others. Level of the fracture (in relation to the lesser trochanter), obliquity of the fracture, and the degree of comminution are used to describe subtrochanteric fractures.
Treatment –
Treatment of subtrochanteric fractures is complicated by the concentration of biomechanical forces in the proximal femur. With weight-bearing, forces in the hip can exceed body weight by many times. In the medial cortex of the subtrochanteric region (1-6 cm below lesser trochanter), a 200 lb man may place 1,200 psi on the bone or fixation devices.
Traction may be used to treat these fractures in very ill or unstable patients. Blade plate or sliding hip screw fixation may be used, but often require very long implants to achieve adequate fixation distally. Cephalomedullary nails, especially in cases with medial comminution and extension above the lesser trochanter, are now used extensively.

