The shoulder is a complex articulation that allows a wide range of positioning of the hand in space. This mobility comes from the numerous articulations in and around the shoulder as well as the ligaments and muscles that control and constrain that movement.
Anatomy –
The term “shoulder” generally refers to the glenohumeral joint, although proper functioning of the shoulder requires the functioning of numerous other articulations. The sternoclavicular joint is the only direct articulation of the upper extremity with the axial skeleton, with the capsular, interclavicular, and costoclavicular ligaments providing stability to this articulation. The clavicle sweeps posterior-laterally in a gentle S-shape, convex anterior medially and concave anterior laterally. A weak tubular middle separates two widened expanses medially and laterally. Laterally, the coracoclavicular ligaments (conoid more medially and trapezoid more laterally) and acromioclavicular ligament suspend the shoulder girdle from the clavicle and resist anteroposterior displacement of the clavicle. Apart form these limited bony and ligamentous attachments, the scapula relies on muscular attachments of the serratus anterior, trapezius, latissimus dorsi, levator scapuli, and rhomboids to provide stability and control its position in space. The glenohumeral articulation is formed by the glenoid of the scapula, a shallow socket deepened by a labrum articulating with the humeral head. This articulation is stabilized by the capsule of the shoulder, the five capsular ligaments (coracohumeral and superior, middle, anteroinferior and posteroinferior glenohumeral ligaments), the muscles of the rotator cuff (supraspinatus, infraspinatus, subscapularis, and teres minor), and the action of the deltoid, biceps, teres major, and pectoralis inserting proximally on the humerus.
A. Clavicle
The clavicle fracture has traditionally been considered an injury that will universally heal with a good result. More recent studies, however, have demonstrated significant disability associated with clavicle fractures, renewing an interest in surgical repair. The function of the clavicle is to function as a strut to maintain the position of the clavicle away from the thoracic cage and maintain optimal muscle length for strength, as well as serving a static suspensory function for the shoulder girdle. Loss of these physiologic functions results in measurable loss of strength in some actions of the shoulder.
History will usually reveal a fall onto the shoulder, a direct blow to the shoulder, or a fall on an outstretched hand. Pain and deformity, as well as ecchymosis may be present. Examination of the skin for tenting over the fracture is important, as the overlying skin may be compromised. Open fractures are rare, but should be identified. Brachial plexus traction injuries should be discovered with a careful neurological exam, and vascular examination should look for the rare subclavian artery injury that may be life- or limb-threatening.
AP radiographs are usually initially obtained, and the diagnosis can usually be made form this view. Specialized views include the apical oblique view for midshaft fractures, serendipity view (or CT scan) for medial fractures, and 10 pound stress view to test the competence of the coracoclavicular ligaments in lateral fractures.
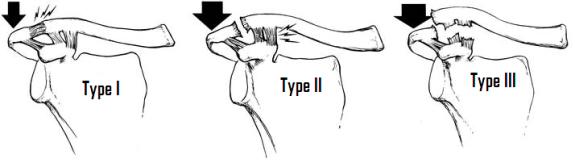
Classification of clavicle fractures generally combines the classification of Allman, which is based on location of the fracture (Type I middle third (~70%), Type II distal third (~20-30%), and Type III proximal third (~3%)), with that of Neer, which subdivides distal third fractures based on the competence of the coracoclavicular ligaments (Type I ligaments intact, Type II conoid detatched from medial fragment but trapezoid intact to distal segment, and Type III with intraarticular extension into acromioclavicular joint).
Treatment of clavicular fractures remains controversial. Some studies have shown non-union rates in adults to be as high as 10-15% with non-operative treatment, while others have shown it to be as little as 0.13%. The majority of Allman Type I clavicle fractures do well with closed treatment, with no difference in outcome between treatment in a sling and figure-of-eight harness until asymptomatic. In cases with significant shortening >2cm, tenting of the skin, open injury, >2cm displacement, floating shoulder, neurologic deficit, and multi-trauma, ORIF with either intramedullary placement of K-wire or screw or plating may be indicated. Allman Type II fractures (especially Neer Type II) have a high rate of non-union with closed treatment, although some argue that these non-unions are asymptomatic. Operative treatment decreases the rate of non-union, and stabilization of the fracture site and reconstruction of the coracoclavicular ligament are the operative goals. Type III fractures are rare, but most seem to do well with non-operative treatment.
B. Acromioclavicular Separations
The acromioclavicular (AC) joint is a diarthroidal joint with a fibrocartilagenous disc interposed between the distal clavicle and the acromion of the scapula. A weak capsule, supplemented by the anterior, posterior, inferior and superior AC ligaments, blends with the deltoid and trapezius fibers superiorly to stabilize the clavicle in the horizontal (anterior to posterior) plane. Vertical stability, critical for the clavicle’s function as a strut suspending the upper extremity, is conferred by the coracoalvicular (CC) ligaments. The CC ligaments, consisting of the conoid ligament medially and the trapezoid ligament laterally, run from the base of the coronoid to the undersurface of the clavicle.
The mechanism of AC joint separations is downward and medial displacement of the scapula by a fall on the “point” of the shoulder or blow to the acromion with the arm adducted. This occurs frequently in sports such as hockey or rugby. The force first disrupts the AC ligaments, followed by the CC ligaments and finally the muscular attachments of the deltoid and the trapezius. This disrupts the suspensory function of the clavicle, allowing the upper extremity to droop (seen on exam and radiographs as an elevation of the clavicle). The patient will exhibit tenderness over the AC joint, pain with longitudinal traction of the arm, and the diagnosis may usually be made with AP and lateral AC joint films.
The classification of clavicle fractures most often used was developed by Rockwell. It describes type I fractures as ligamentous strains of the AC ligaments. Rupture of the AC ligaments with injured but intact CC ligaments results in a type II separation. Type III separations are complete AC and CC separations with 25-100% inferior displacement of the acromion based on the measurement of the coracoclavicular clear space. Posterior, >100% inferior, and anterior or subcorocoid dislocations are types IV, V, and VI respectively.
Type I and II fractures are treated symptomatically in a sling for 10-14 days, followed by limiting of heavy lifting and contact sports for 8-12 weeks. Type III fractures may usually be treated non-operatively following the above protocol, but in heavy laborers, overhead motion athletes, and patients with a brachial plexus palsy they may progress to surgical treatment. Types IV, V, and VI usually require operative ORIF, with smooth K-wires passed through the AC joint or coracoclavicular reconstruction using a screw or wire.
C. Scapula Fractures
Scapular fractures are rare injuries, usually associated with high-energy trauma, such as MVA and motorcycle accidents, and may occur after direct blow to the scapula, axial loading of arm, or avulsion of a muscular insertion. As high-energy fractures, they are associated with a high incidence of associated injury, including pneumothorax (11-38%), fractured ribs (27-54%), pulmonary contusion (11-54%), clavicle injury (23-39%), brachial plexus palsy (5-13%), and skull fractures (24%). Overall mortality rate may be as high as 15% due to the significant associated injuries.
Radiographs should include an AP chest (to look for rib fractures, pneumothorax, and contusion), a true AP of the scapula, and a scapular-Y view will demonstrate body fractures as well as acromial fractures. The axillary view is helpful for evaluating glenoid fractures (and ensuring that the humeral head is located), and the cephalic tilt or Stryker notch view is useful for coracoid fractures. Non-fused ossification centers in the scapula, especially the os acromiale, may be confused with fracture.
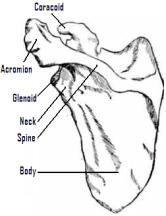
Although many classifications have been described for each of the subsets of scapular injuries, most fractures of the scapula are described by anatomic location (body, spine, glenoid, neck, coracoid, and acromion).
Treatment of scapular fractures varies by anatomic area. Intraarticular glenoid fractures may be treated with ORIF, especially if they are large (25% of joint surface) or associated with instability. Nondisplaced acromion fractures respond well to symptomatic treatment in a sling, but displaced fractures should undergo ORIF with tension banding. Coracoid fractures may be treated non-operatively unless associated with AC joint separation, then requiring ORIF of the AC joint or both. Scapular body fractures are best treated non-operatively with ice and immobilization. Glenoid neck fractures may be treated symptomatically in a shoulder immobilizer with early range of motion, unless associated with a clavicle fracture (“floating shoulder”); then, ORIF of the clavicle is indicated.
D. Shoulder Dislocations
The remarkable mobility of the shoulder also makes it prone to instability with disruption of the normal function of the capsule, ligaments, tendons, and muscles that hold it in place. Dislocation of the shoulder is a dramatic event that requires prompt action to reduce the acute and chronic morbidity associated with this relatively common problem.
There are two main patterns of glenohumeral dislocation – anterior and posterior. In an anterior dislocation, the arm is often forced into abduction, extension and external rotation. This stresses the anterior capsule and capsular ligaments, and when these fail, the humeral head comes to lie on the anterior-inferior lip of the glenoid. The humeral head may be palpable anterior to the AC joint. A posterior dislocation may occur through axial loading of a adducted, internally rotated arm or with a direct blow to the anterior shoulder. It may also occur with violent contraction of the muscles of the shoulder, as occurs in electrocution or seizure. In these cases, the internal rotators overcome the external rotators and force the head out of the glenoid posteriorly. This may be seen as a hollow beneath the acromion.
A rare variant of anterior dislocation is the luxatio erectae, in which the arm is maximally abducted and sees an axial loading force, causing an anterior and inferior dislocation. The arm will be locked in this maximally abducted position, requiring special reduction maneuvers.
History of these injuries should include a detailed mechanism, including the direction and amount of force that was required to dislocate the extremity. A history of previous dislocation and any treatment received is also valuable. On exam, severe pain and muscle spasm is the rule. A complete neurovascular exam to rule out axillary nerve or brachial plexus injury should be documented.
Radiographic evaluation of these injuries requires a minimum of two views, commonly an AP and an axillary lateral. If the arm cannot be abducted enough to obtain an axillary lateral, a Velpeau axillary lateral (shot from vertical while the patient leans 30 degrees backwards over the cassette) or a West Point axillary lateral (patient prone, cassette superior to shoulder, x-ray beam centered at axilla, 25 degrees downward from horizontal and 25 degrees medial) may be taken as a second view.

Prompt reduction of acute dislocations reduces the potential morbidity by taking the stretch off of the neurovascular structures, decreases the extent of bony defects in the soft humeral head, decreases the muscle spasm that must be overcome to achieve reduction, and increases patient comfort dramatically. Administration of narcotics and muscle relaxants aids in the reduction, as voluntary relaxation of the muscles in spasm may not be possible. Although many different reduction techniques are described, the Hippocratic technique of traction/counter-traction and gentle internal and external rotation is still effective and frequently used. Following reduction, repeat neurovascular exam, repeat radiographs to confirm location, and placing of the patient in a sling is the treatment of choice (the position of the arm, internal vs. external rotation is debated). Range of motion of the elbow, wrist and hand during sling treatment is important. Sling treatment for 6 weeks with graduated liberalization of flexion and external rotation is followed by isometric strengthening therapy.
Instability of the shoulder may result following dislocation, especially multiple dislocations or those associated with a Hill-Sachs lesion (a bony defect on the posterior portion of the humeral head from the impact of the glenoid) or a Bankart lesion (an anterior glenoid defect). Chronic instability may require stabilization procedures after recovery form the acute trauma.
E. Proximal Humerus Fractures
Proximal humeral fractures represent 2-3% of fractures of the upper extremity. This fracture often occurs in older, osteoporotic women, adding a level of complexity to the treatment.
The humeral shaft joins the proximal humerus at the surgical neck, just below the greater and lesser tuberosities at the metaphyseal flare. The anatomic neck lies between the tuberosities and the articular surface of the proximal humerus and is the site of insertion of the capsule. The muscles of the rotator cuff insert on the tuberosities; supraspinatus, infraspinatus, and teres minor insert on the greater tuberosity and subscapularis on the lesser tuberosity. These tuberosities are separated by the bicipital groove, within which lies the tendon of the long head of the biceps and the arcuate artery (a branch of the anterior humeral circumflex artery). The bicipital groove is traversed by the transverse humeral ligament. The blood supply to the head is tenuous – the anterior humeral circumflex artery (a branch of the axillary artery) sends the arcuate artery to anastamose with the posterior humeral circumflex artery. This ascending connection provides the main arterial supply to the head, and can be completely disrupted with a four-part fracture, leading to avascular necrosis. The brachial plexus and axillary artery pass below the coracoid and along the anterior inferior glenohumeral joint capsule to enter the arm.
Proximal humerus fractures may occur by high energy mechanisms in young people or low energy in older, osteoporotic people. Most commonly, a fall on the arm is the mechanism of fracture, although direct trauma, and forceful muscular contraction (electrocution of seizure) may cause this injury. The muscular attachments cause separation of the fracture fragments – the shaft is drawn anterior and medially by the pectoralis major; the greater tuberosity may be pulled posteriorly and superiorly by the infraspinatus and supraspinatus, respectively; the subscapularis draws the lesser tuberosity medially, internally rotating the head fragment if attached.
The patient will present with a painfully swollen arm. This may obscure associated injuries to the face, neck, or chest wall. A careful neurovascular exam, including axillary nerve testing by examining for cutaneous sensation of the lateral shoulder, should be documented.
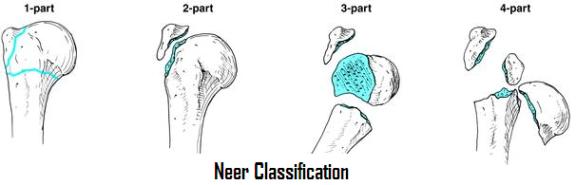
Radiographs should include AP and scapular-Y views, as well as an axillary lateral or Velpeau view. The Neer classification is most frequently used for proximal humerus fractures, dividing fractures by the number of displaced principal fragments (head, shaft, greater tuberosity, lesser tuberosity), defined as 1cm or greater displacement of a fragment or rotation of 45 degrees or greater. Two part fractures have one displaced fracture line, commonly surgical neck fractures or greater tuberosity fractures. Three part fractures usually have a surgical neck fracture and tuberosity fracture with one tuberosity remaining attached to the head piece. Four part fractures have a surgical neck fracture, separation of the tuberosities, and a head fragment.
Simple, non- or minimally displaced proximal humerus fractures may be treated closed. In active people, less than 5mm superior or 10mm posterior displacement of the greater tuberosity, less than 50% shaft displacement, and less than 45 degrees angulation are relative indications for non-operative treatment. In older, less active people, more displacement (1cm superior displacement of greater tuberosity, any cortical contact of the shaft) may be acceptable. Closed treatment should consist of a sling for one to two weeks, with immediate elbow, wrist and hand motion. Pendulum exercises may begin at two weeks, assisted range of motion at 3-4 weeks, and formal therapy at 6 weeks. Surgical treatment for these minimally displaced fractures may be indicated with ipsilateral neurovascular injury, open fractures, or multiple trauma.
Displaced fractures may be treated by a variety of surgical means. Closed reduction and percutaneous pinning of surgical neck fractures is often effective. Open reduction and internal fixation may be used to treat two part surgical neck, three, and even four part fractures in a young person. Greater tuberosity fractures may be sutured into place with purchase in the rotator cuff, and suture repair may be used through drill holes in three and four-part fractures or combined with an Enders nail. Hemiarthroplasty or total shoulder arthroplasty may be indicated in four part fractures or fractures with an articular split.
Complications seen after proximal humerus fractures include instability, malunion, non-union, avascular necrosis of the humeral head, infection, neurovascular injury, arthritis, impingement, and rotator cuff tears.

