Reattachment or replantation of a severed hand digits is frequently indicated. Factors affecting the decision to perform replantation include the level of amputation and the nature of injury along with the patient’s age, occupation, medical history, and associated risk factors. The most common amputation injury results from power saws. The mechanism of amputation and the resultant injury affect the surgeon’s decision to attempt replantation versus revision amputation. Clean-cut or sharp amputations are favorable for replantation. Crushing and avulsion injuries are less likely to be salvageable. Most replantations should be attempted in children and young adults because these patients have a greater propensity for regeneration of nerves and less propensity for joint stiffness. Good function can be expected with replantation at the wrist and distal forearm level. The thumb, which is vital for optimal hand function because of its location on a separate plane from the fingers, is always replanted if possible. Multiple finger amputations should be replanted as well as single digits if the amputation is distal to the insertion of the FDS tendon.
Indications
Because the final decision regarding replantation rests with the patient and the surgeon, there are no absolute indications for replantation of an amputated part. The following discussion reflects our present practice combined with the published recommendations of the previously noted authors. The factors discussed should be taken as relative guides based on current knowledge and experience.
Age
Replantations have been reported in patients a few weeks old and in those older than 70 years. The young patient poses particular problems, especially regarding digital replantations, because of the increased technical difficulty in microvascular anastomoses of their smaller digital vessels. Postoperative anxiety may contribute to vasospasm, and rehabilitation of children may be less predictable than of adults. Nevertheless, quite satisfactory functional results have been reported, and most authors consider replantation over amputations of almost any part including lower extremity parts in children.
The upper age limit beyond which replantation should not be considered has not been clearly established. Poor nerve regeneration and joint stiffness are factors that limit the functional outcome. Replantation above the elbow, through the elbow, or through the proximal forearm results in little promise for hand function in the elderly; however, the elbow in above-the-elbow amputations may be preserved in anticipation of a subsequent below-the-elbow reamputation to allow more satisfactory prosthetic fitting. Because the potential for return of sensibility and motion is better after replantation at and beyond the tendinous portion of the forearm, older patients may be considered as serious replantation candidates if their injury is more distal.
Severity of Injury
The types of injuries that have the best outlook regarding survival and return of function after replantation include (1) clean, sharp “guillotine” amputations, (2) minimal local crush amputations, and (3) avulsion amputations with minimal proximal and distal vascular injury. Ideally, significant additional injury to the limb should not be present, especially of the vessels, proximally and distally. Crushed and avulsed vessels require debridement and the use of interpositional vein grafts as needed. Ring avulsion-degloving injuries may be revascularized and salvaged; however, if the skin has been completely degloved or if the digit has been amputated, vein grafts may be required and the outlook for useful function is extremely uncertain.
Level of Injury and Part Amputated
Amputations through the humerus, elbow, and proximal forearm have the potential for successful replantation and useful function, especially in a young, healthy patient and especially if the injury is clean and sharp. The patient should be young enough and motivated enough to be able to await nerve regeneration sufficient for return of function. Replantation more distally, whether through the distal forearm, wrist, metacarpals, or digits, also should be seriously considered because, generally, the potential for sensory and motor return is good.
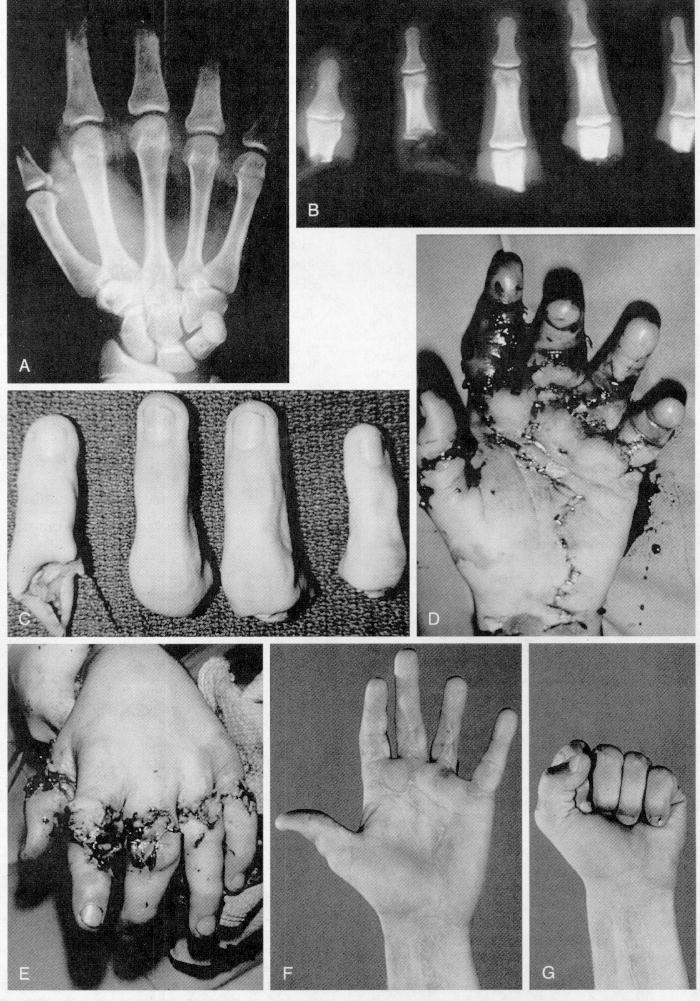
Thumb amputations at almost any level should be considered for replantation in spite of nerve and tendon avulsion and joint involvement. If the thumb can be revascularized, sensibility can be restored with nerve grafts or a neurovascular island pedicle transfer if needed, and motion can be achieved with tendon grafts or transfers. Replantation of single and multiple digits distal to the flexor digitorum sublimis insertion should be expected to achieve satisfactory function ( Fig. 60-16 ). Although many patients do well without replantation of single-digit amputations, such a replantation may be worthwhile for some musicians, those with other special occupations, some children, and for other aesthetic or social reasons. Replantation of a single digit also may be helpful if the remaining attached digits are severely damaged, especially with tendon and nerve injury over the proximal phalanx.
If multiple digits have been amputated, replantation of at least two digits in the long and ring positions provides a good combination of digits to use with the thumb for pinch and for power grip.
In bilateral amputations, replantation on each side should provide better function than bilateral prostheses. If replantation is not suitable or possible because of extensive injuries on one side, the best side should be selected, and at times parts from one side may be attached to the opposite, more suitable stump.
Although amputations through the joints impair the movement of those joints, a satisfactory limb can result through arthrodesis, excisional or fascial arthroplasty, or,in ideal circumstances, silicone implant arthroplasty.
Warm Ischemia (Anoxic) Time
Because irreversible necrotic changes begin in muscle after 6 hours of ischemia without cooling (at 20° to 25° C), it is preferable to begin the replantation of parts amputated proximal to the palm within this time. With cooling (to 4° C), this time may be extended up to 12 hours. For parts with no muscle (digits) the allowable warm ischemia time may be 8 hours or more. With cooling this has been extended to longer than 30 hours.
Contraindications
Contraindications to replantation include medical conditions that are not compatible with a long duration of anesthesia. Relative contraindications include vascular disorders, diabetes, hypertension, multiple injury levels, extreme gross contamination, some ring avulsion injuries, prolonged ischemia, and advanced age. In border-finger amputation (index and small fingers), replantation is often unnecessary because a three-finger hand is both functionally and aesthetically acceptable. There is a high rate of adhesion formation and resultant stiffness in zone II replantations as a result of the presence of two tendons in the flexor tendon sheath. Before granting informed consent, the patient must be informed of the many months of postoperative care and rehabilitation that are required after replantation. Although contraindications may seem to be defined more easily than indications, each patient must be evaluated individually with advantages and disadvantages considered before rejecting a given situation as hopeless.
Age
As noted previously, age alone is not a contraindication to replantation. Although older patients may obtain satisfactory function after replantation of fingers, thumbs, and hands, rarely do they achieve adequate sensibility, forearm and hand muscle strength, and coordination sufficient to warrant replantation of more proximal amputations. The patient’s physiological status, the presence of other diseases, and general level of activity should also weigh heavily in the evaluation.
Severity of Injury
Despite dramatic results that have been achieved using long vein grafts to salvage limbs, extensive crushing, avulsing, and segmental injuries at multiple levels damage the distal vascular tree sufficiently to frequently defeat replantation attempts. This is especially true in such digital injuries. Ring avulsion amputations through the joint are usually best treated by closure of the amputation.
Injuries contaminated extensively with soil, especially from the barnyard, carry a high risk of significant infection and should be evaluated carefully before replantation.
Level of Injury
Because of the slowness and unpredictability of nerve regeneration and the muscle atrophy and joint stiffness that develop, replantation near the shoulder generally carries a poor prognosis regarding hand function. Replantation for salvage of the elbow for later below-the-elbow prosthetic fitting may be feasible in selected patients. Replantation just above the elbow, through the elbow joint, or in the proximal forearm also carries a guarded prognosis, especially in older patients because of questionable nerve regeneration, limitation of elbow motion, and persistence of intrinsic muscle atrophy; however, younger patients may benefit from replantation at these proximal levels, especially if the injury is sharp and clean.
Skeletal muscle undergoes irreversible necrotic changes after about 6 hours of total warm ischemia. These changes can be slowed or minimized if the part is cooled to near 4° C. Although replantation of parts containing small amounts of muscle, such as the hand, probably is less risky, larger parts such as the forearm and arm above the elbow should probably not be replanted if they cannot be revascularized between 6 and 8 hours after amputation. The risk of renal damage resulting from myoglobinuria, acidosis, and hyperkalemia is increased after the replantation of a part with significant amounts of necrotic muscle. The risk of infection also is greater, and the long-term outlook for a functional limb is poor.
Digital viability also can be prolonged by cooling to 4° C. Because the amount of skeletal muscle in digits is not significant, the risk to the patient is minimal if digits are replanted. Cooled digits have been replanted successfully at 30 hours and more after amputation.
If amputated parts have been frozen, placed in nonphysiological solutions such as formaldehyde or alcohol, or allowed to dry excessively, the chance of survival is so low that replantation attempts are futile.
Preexisting Deformity or Disability
If the amputated part was already deformed or disabled because of some congenital or acquired disorder, satisfactory function is unlikely to be achieved by replantation. Conditions that would fit this situation include, but are not limited to, scar deformity and contracture caused by previous burns or mangling injury, significant residual deficits from spinal cord
Other Conditions That Might Preclude Replantation
In the same accident that causes the amputation of a part, patients at times sustain significant intracranial, thoracic, cardiovascular, or major intraabdominal visceral injuries requiring lengthy life-saving operations. In such circumstances a major limb replantation may not be possible because of excessive ischemia time. Digits may be cooled to 4° C in a refrigerator and saved for replantation later if technically feasible and if the patient’s condition permits.
Patients with preexisting diseases that typically affect peripheral blood vessels are probably poor replantation candidates, especially if their vessels have an unsatisfactory appearance when inspected under the operating microscope. Patients with diabetes mellitus, rheumatoid arthritis, lupus erythematosus, other collagen vascular diseases, and significant atherosclerosis fit into this category.
Severe chronic or uncompensated medical illnesses such as coronary artery disease, myocardial infarction, peptic ulcer disease, malignant neoplasms, and chronic renal or pulmonary disease may increase the anesthetic risk enough to preclude replantation.
Considerable judgment is required when assessing patients with psychiatric illnesses who have amputated parts. If the amputation event is an act of self-inflicted mutilation or attempted suicide during a psychiatric episode that can be treated and stabilized, replantation carries considerable risk of failure. If the amputated part is a focus in the patient’s mental illness, it is likely that the part, if replanted, will be reinjured. If the amputation occurs as a true inadvertent accident, especially in a patient whose mental illness is compensated, the outlook for replantation might be better. Valid psychiatric evaluation of patients with amputated parts in an emergency room is extremely difficult. The inability of patients with profound psychiatric illness to understand their delicate postoperative condition and to cooperate with the difficult rehabilitation process further complicates their care as replantation patients. VanderWilde et al. reported successful treatment of a 15-year-old girl with a self-inflicted incomplete wrist disarticulation that resulted in amputation. Because the child was a minor and the family desired replantation, the procedure was attempted after 54 hours of cold ischemia time. At follow-up after replantation and reconstructive procedures, the patient demonstrated complete range of passive finger motion and ability to grasp and use the hand for assisted functions in activities of daily living. Her psychiatric status remained stable, and no further injuries were reported.
Preparation of Limb
The severed part is cleansed, placed in sterile gauze, placed in a sealed bag, and bathed in ice water until replantation. Major amputations are those involving a large muscle mass, which tolerates shorter periods of ischemia. Salvage time can be increased to 12 to 16 hours by cooling and reperfusion if initiated early in the course of replantation. Reperfusion is accomplished by cannulating the arterial inflow vessel in the amputated part and infusing autologous blood and heparin solution. In minor replantation (e.g., digital replantation), 18 to 30 hours of cool ischemia is tolerated.
Repair is sequential (Figure below). In digital replantation, the approach is made through a modified Bruner incision palmarly and a straight midline incision on the dorsum. The amputated part is prepared on a separate table as the patient is prepped. After cleansing and debridement, veins, arteries, and nerves are identified and tagged. Bone fixation is followed by the repair of flexor tendons, digital arteries, digital nerves, extensor tendons, dorsal veins, and skin. If there has been prolonged ischemia time, the arteries can be repaired earlier in the sequence. Special instrumentation is necessary, including magnifying loupes, an operating microscope, and microvascular instruments. Injuries with segmental loss of structures require bone shortening. Interpositional vein and nerve grafts can be used to bridge vessel and nerve gaps. The palmar forearm and dorsal foot are excellent donor areas for vein grafts, whereas the posterior interosseous nerve at the wrist, lateral antebrachial cutaneous nerve, and sural nerves are used for nerve grafts. Anatomic parts from nonreplantable digits can also be used for salvaging the more functional digits.
After revascularization, soft tissue defects may require coverage with skin grafts or microvascular free flaps. Flaps that are frequently used include the lateral arm, scapular, radial forearm, latissimus dorsi, and other muscle flaps.
A bulky, noncompressive, well-padded dressing and splint are applied for postoperative protection and comfort. The patient is informed of the deleterious effects of tobacco and cold exposure that include arterial thrombosis. Analgesics, hydration, and anticoagulants are used. A mixture of 5000 units of heparin and 500 ml of low-molecular-weight dextran is given at a rate of 30 ml/hr. Prothrombin time and partial thromboplastin time are monitored.
Post-replantation monitoring
Clinical examination remains the most reliable monitoring technique. Venous congestion may be indicated by swelling, blue discoloration, and dark blood on pinprick analysis. Treatment includes releasing tight dressings and sutures, removing the nail plate and applying heparin-soaked pledgets to the nail bed, and applying medicinal leeches. Leeches remove venous blood and inject hirudin, an anticoagulant. Blood loss should be monitored when using leeches. Antimicrobials are given to protect against infections caused by Aeromonas hydrophila.
Arterial occlusion is suggested by coolness to touch, loss of tissue color, and loss of skin turgor. If occlusion is clinically established, urgent surgical correction should be performed to salvage the severed part. In our experience, reoperation can salvage half of cases
TABLE — Replantation of the Amputated Extremity
Indications
Relative Contraindications
Young stable patient
Single digit, unless thumb
Thumb
Avulsion injury
Multiple digits injured
Prolonged warm ischemia (≥12 hr)
Sharp wounds with little associated damage
Gross contamination
Upper extremity (children)
Prior injury or surgery to part
Absolute Contraindications
Emotionally unstable patients
Associated life threats
Lower extremity
Severe crush injuries
Inability to withstand prolonged surgery
*If the victim is a child or if there are multiple losses, salvage replantations are attempted, and the relative contraindications are ignored.
Figure: Sequence of replantation
A, Radiograph of hand with multiple-digit amputation. B, Radiograph of severed digits. C, The severed digits with fairly sharp amputation edges. D, Immediately after replantation (palmar view). E, Immediately after replantation (dorsal view). F, Three-year follow-up showing extension. G, Three-year follow-up showing flexion.