Overview
Stress fractures are common athletic overuse injuries. Although there are numerous risk factors that contribute to the development of stress fractures, they generally result from repeated overloading of the bone that exceeds its remodeling capability. Most stress fractures occur in the lower extremity. Common sites for stress fractures include the tibia, fibula, metatarsals, tarsal navicular, calcaneus, and femoral neck. Upper extremity stress fractures may occur in repetitive activities such as baseball and racquet sports. Stress fractures of the ribs have been reported in rowing sports and golf. Spine stress fractures are seen in gymnasts.
History/Physical Examination
Localized pain on exertion is the primary complaint with a stress fracture. Patients often report a recent increase or change in training activity. Symptoms usually improve with rest. It is important to ask about previous stress fractures, as 60% of patients with stress fractures have had a previous stress fracture. A detailed history of the patient’s health, medications, and personal habits should be obtained to rule out factors that may increase the risk of stress fractures.
Tenderness to palpation is present at the injury site and is one of the most consistent physical examination findings. Soft tissue swelling may be seen.
Risk Factors for Stress Fractures
- Sports involving running and jumping
- Rapid increase in physical training program
- Poor pre-participation physical condition
- Female gender
- Hormonal or menstrual disturbances
- Low bone turnover rate
- Decreased bone density
- Decreased thickness of cortical bone
- Nutritional deficiencies (including dieting)
- Extremes of body size and composition
- Running on irregular or angled surfaces
- Inappropriate footwear
- Inadequate muscle strength
- Poor flexibility
Imaging
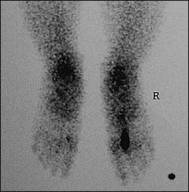
Once a clinical diagnosis of a stress fracture has been made, there are numerous imaging modalities that may be used to confirm the diagnosis. Radiographs should be obtained although stress fractures may not be seen for as long as 2-10 weeks after the onset of symptoms. Findings on a plain radiograph that may indicate a stress fracture include periosteal bone formation, sclerosis, callus, or a fracture line. A triple phase bone scan is helpful in the early diagnosis of a stress fracture. It is an extremely sensitive test but non-specific test for the workup of stress fractures. A CT or MRI may be helpful in further localizing the injury.
Bone scan: stress fracture of the 2nd metatarsal
Treatment
In general, most stress fractures are treated conservatively. First it is important to identify and correct the causes of the stress fracture. Non-operative therapy includes non-steroidal anti-inflammatory drugs, cryotherapy and activity modification. Treatment includes modified activity for 4-8 weeks until pain-free. Activities of daily living are permitted but impact or repetitive activities are avoided. Cross training and non-weight bearing aerobic activity is encouraged. Once pain has resolved, then a gradual return to the offending exercise is permitted.
There are certain stress fractures that are more concerning and tend to require surgical treatment more frequently. The more common high-risk stress fractures include the anterior tibia, femoral neck, tarsal navicular, and the proximal fifth metatarsal. Less common high risk stress fractures include patella, medial malleolus, talus, and great toe sesamoid fractures.
Anterior Tibial Stress Fractures
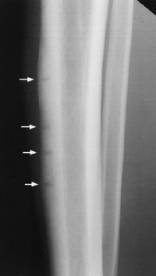
Most tibial stress fractures occur in the posteromedial cortex and may be treated non-operatively. However, anterior tibial stress fractures of the midshaft are more concerning and may progress to a non-union or complete fracture. These injuries are common in repetitive jumping activities. This area is prone to complications because the anterior tibia is the tensile side and it has a relative lack of a blood supply. One radiographic finding that signifies a poor prognosis is the “dreaded black line” of the anterior cortex. This radiographic finding signifies a limited ability to heal. These fractures may be treated initially with non-operative management but may require further operative treatment with intramedullary stabilization.
Anterior tibial stress fractures: the “dreaded black line”
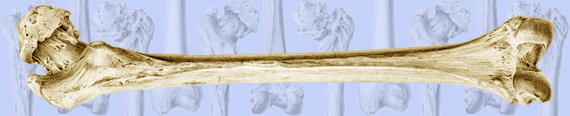
Femoral Neck Stress Fractures
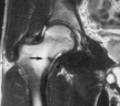
MRI showing compression sided femoral neck stress fracture
Patients will present with anterior groin pain. The pain often leads to an antalgic gait. On physical examination, palpation of the fracture is often difficult due to the amount of overlying soft tissue; however, pain can be elicited by internally and externally rotating the hip joint. Stress fractures can occur on either the compression or tension side of the femoral neck. Compression type fractures are treated mainly with non-operative management. It is the tension sided stress fractures that are more worrisome. Tension sided fractures have a grater risk of progressing on to a displaced femoral neck fracture. Surgical treatment with femoral neck pinning should be pursued for tension sided stress fractures, compression fractures involving greater than 50% of the femoral neck, and displaced fractures.
Tarsal Navicular Stress Fractures
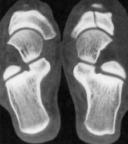
Bone scan and CT scan: tarsal navicular stress fracture
Tarsal navicular stress fractures are common in jumping and running sports. Patients will present with medial foot pain. If diagnosed early, these injuries may be treated with non-weight bearing in a cast for 6-8 weeks. Displaced fractures or non-unions should be treated with open reduction/internal fixation and bone grafting.
Proximal Fifth Metatarsal Stress Fractures
Proximal 5th metatarsal stress fracture treated with compression screw fixation


Stress fractures of the fifth metatarsal occur at the proximal diaphysis. Stress fractures in this area have a high risk of non-union and are at high risk or refracture in the athletic population. Acute injuries tend to do well with non-weight bearing immobilization for 6 weeks. Compression screw fixation has been advocated for patients failing non-operative management and high-level athletes.