Metastatic bone lesions are the predominant malignancy to effect bone, with 15 times the occurrence rate of the next most common bone malignancy. There are 5 tumors notorious for their capacity to spread to bone that include Breast, Lung, Thyroid, Renal Cell and Prostate (a popular memory aid is BLT Kosher Pickle.) Primarily they spread to spine, but lung cancer is known to metastasize to the peripheral extremities. Only 9% of the time is a single metastasis detected.
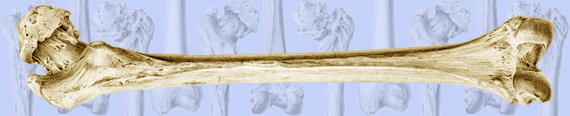
Symptoms are variable depending on the site, type and size of the lesion. Blastic metastases are usually non-painful and likely relates to the decreased risk of pathologic fracture when compared to lytic metastases. Hypercalcemia is not uncommon, especially with breast and lung metastases. For the most part breast lesions are blastic but the other lesions are more variable (Figure 17).
Figure # 17
Blastic metastases to the pelvis and proximal femur
eduserv.hscer.washington.edu
From the orthopedic standpoint, pathologic fractures forebode an average survival of 19 months depending on the type of lesion with the worst average survival with lung metastases being an average of 4 months. Before any intervention is to be undertaken a minimum life expectancy of 6 weeks should be expected. The most common lesion about the hip occurs at the intertrochanteric region and should be treated with a long-stem, calcar-replacing arthroplasty. The next most common lesion of the hip involves the femoral neck and should be treated with a cemented bipolar. Femoral shaft lesions should be treated with a cephalomedullary device to protect the femoral neck and intertrochanteric region if the metastasis spreads. As previously stated, isolated metastases are uncommon and radiographs of the entire bone to be treated must be taken to confirm the absence of other lesions that could compromise surgical interventions. For example, an intertrochanteric lesion to be treated with a long stem arthroplasty would suffer catastrophic failure if a second missed lesion were to be present at the distal extent of the arthroplasty stem causing a large stress riser and eventual periprosthetic fracture. Lesions of the spine have different characteristics depending on location. Cervical spine metastases are rarely problematic due to the wide canal with relation to spinal cord diameter. Thoracic spine lesions, on the other hand, are well known to cause paralysis due to the narrow canal with relation to a flare in the spinal cord diameter. These lesions should be treated with a thoractomy, vertebrectomy, and placement of a femoral allograft with cement. This is one of the few indications for allograft when dealing with metastatic lesions, as most lesions will require post-operative XRT rendering bone graft non-viable. In this case, the femoral allograft acts as a structural graft to prevent collapse without the hope of bony integration. Low thoracic and lumbar vertebra can also progress to paralysis, though the canal to cord diameter ratio is more favorable. These lesions should also be approached anteriorly to perform vertebrectomy with placement of femoral allograft and cement. A posterior approach with laminectomy to decompress the cord is a tempting option but should be resisted for fear of further destabilizing the spine. In many cases, the intact posterior elements provide the only resistance to complete mechanical failure of the bone. Acetabular lesions are some of the most challenging metastases to treat. In general they are treated with hip arthroplasty after the lesion has been removed with a curette and replaced with cement that contains structural metal rebar reinforcement.
Special mention of pre-operative planning in the case of renal cell carcinoma metastasis needs to be made. As one would expect from the tissue of origin, these lesions are highly vascular. Exposure during attempts to remove or biopsy these lesions can cause exsanguination in a matter of moments. For this reason, pre-operative angioablation should be performed.
As previously mentioned, XRT is often used in conjunction with the above measures. Prostate metastases and lymphoreticular lesions are the most radiosensitive; while breast is intermediately sensitive. Tamoxifen is only 30% effective against breast cancer metastases unless they are known estrogen receptor positive in which case the effectiveness increases to 70%. Finally, renal and GI metastases are the least radiosensitive.