Introduction
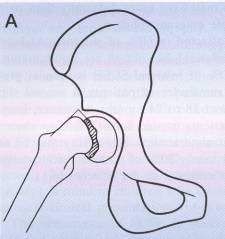
SCFE occurs through the unfused growth plate of the proximal femur where the femoral head slips posteriorly on the femoral neck. Serious consequences of the problem, such as gait disturbance, post-traumatic arthritis, chondrolysis and osteonecrosis of the femoral head can occur, leading to lifelong disability. Prompt diagnosis and treatment of this problem is essential.
Presentation
SCFE occurs in children averaging 12 years in girls and 13-14 years in boys. More than 60% of SCFE patients are in the 90th percentile for weight. Patients present with thigh, knee or hip pain and often an antalgic, out-toed gait. Nearly 85% have had pain at least three weeks at the time of presentation (so called chronic slips) and are able to weight-bear. The ability to weight-bear makes the SCFE stable by Loder’s criteria, which has profound prognostic significance. More rare, and much more serious are those children who have acute onset of severe pain and are unable to weight-bear, even with the use of crutches; the unstable slip. These acute events can either occur spontaneously or in the face of chronic pain with an abrupt incident, the so called ‘acute on chronic’ slip.
Pathophysiology
Instability of the proximal femoral physis can be caused by numerous etiologies. The orientation of the proximal femur, joint reactive truss across the physis and the physis’ intrinsic strength are all factors. Retroversion of the proximal femur (as noted by outward > inward rotation) stresses the physis more than normal biomechanics. Large body weight can markedly increase joint reactive forces, and this combined with retroversion or some intrinsic physeal weakness can increase the risk of slip.
Intrinsic strength of the physis can be altered by rapid or abnormal growth, as with those children on growth hormone or with other endocrine abnormalities. Children with renal osteodystrophy or hypothyroidism are at increased risk of developing SCFE: if one side slips the risk of the contralateral hip slipping approaches 100%. Children who are younger than the expected age (i.e., 12 years) when they suffer SCFE should be carefully evaluated for endocrinopathy.
Diagnosis
Children with SCFE are of preteen or adolescent age, frequently obese and present with out-toeing, limp and pain in the thigh or hip. SCFE is more common in Blacks and Polynesian children.
On physical exam there is often a decrease in flexion of the affected hip with an obligate outward rotation of the hip as it is brought into flexion.
Radiographs changes are diagnostic but, especially with slight or early slips, can be subtle. The frog lateral is more sensitive for diagnosis than the AP pelvis, as a slight offset of the epiphysis on the neck may be visible before the AP appears abnormal. A few subtle signs do exist on the AP radiograph. Klein’s line is a line drawn above the superior femoral neck, this should intersect the lateral edge of the epiphysis. In SCFE, as the femoral head slips posterior to the femoral neck, Klein’s line passes lateral to the femoral head, either not intersecting it at all, or less than on the contralateral side. The Blanche sign is seen on the AP pelvis at the lateral physis/metapohysis junction as a slight increase in radiodensity (whiteness) due to the overlap of the metaphysis and epiphysis. In very early or “pre-slip” stage, the only finding may be a widening of the proximal femoral physis compared with the contralateral side.
Classification
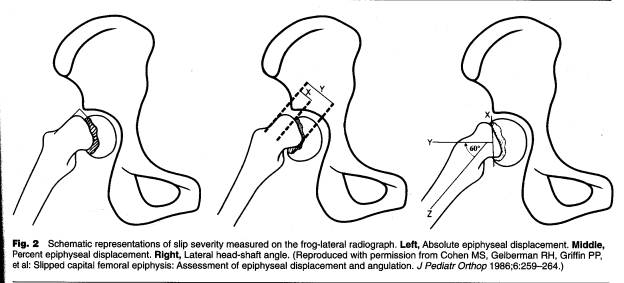
In addition to timing of the slip (acute, chronic or acute on chronic) or the stability of the slip (stable – able to be walked on with or without crutches or unstable – unable to ambulate) the severity of the slip can also be classified. The severity is graded by either percent epiphyseal displacement or lateral head-shaft angle; both are measured on the frog lateral. A slip angle or percentage less than 30º (or %0 is mild, 30-50 moderate and >50º (or%) severe.
Treatment
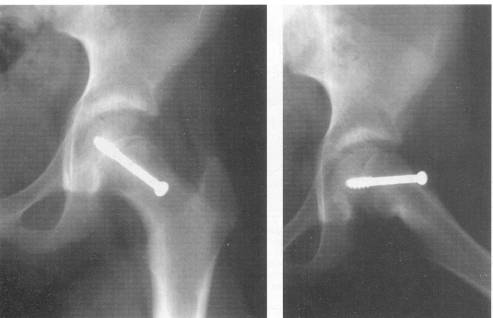
Open bone-peg epiphysiodesis, spica cast immobilization and multiple pin fixation have all fallen out of favor in recent years for the safer single cannulated 6.5 or 7.3 mm screw fixation in situ. This technique utilizes Carm views of the affected hip to place a screw into the center of the epiphysis on both the AP and lateral planes, perpendicular to the physis and no closer to subchondral bone than 5 mm. [The treatment is aimed at closing the proximal femoral physis to avoid future slip]. After the screw is placed, a range of motion is checked (“approach and withdrawal”) using C-arm to assure the screw does not exit the femoral head on any view.
Fixation of the contralateral hip is justified with radiographic changes, pain consistent with SCFE or endocrinopathy. The actual incidence of idiopathic bilateral SCFE ranges in the literature from 22% to 80%. Prophylactic pinning of the contralateral hip in idiopathic SCFE has proponents, but at this point is still controversial.
Complications
Osteonecrosis of the femoral head is a devastating complication in this adolescent age group, often necessitating hip fusion or replacement.
A stable slip should have very low risk (<5%) of this complication, but an unstable slip is at risk nearly 50%. The family must be made aware of the pre-operatively, and also understand the importance of receiving immediate care if pain arises on the contralateral hip, so as to avoid an unstable slip on the other side. The role of reduction of the SCFE at the time of screw fixation and its impact on the rate of osteonecrosis (ON) is a highly controversial topic. For years “incidental” reduction of unstable slips was the only type of reduction described for fear that the surgeon would be held responsible for ensuing ON of the hip if the reduction was viewed as intentional. In fact bone scan studies done before operative intervention have shown that in unstable hips loss of blood supply occurred at the time of the slip, not at the time of surgery. Over the past five years reduction of unstable slips has been better accepted, although “in situ” screw fixation is still better accepted. Forceful manipulation, however, is never acceptable.
Chondrolysis, or loss of articular cartilage following SCFE is a somewhat mysterious event.
It is known to increase after spica casting or multiple pin penetration in the joint.
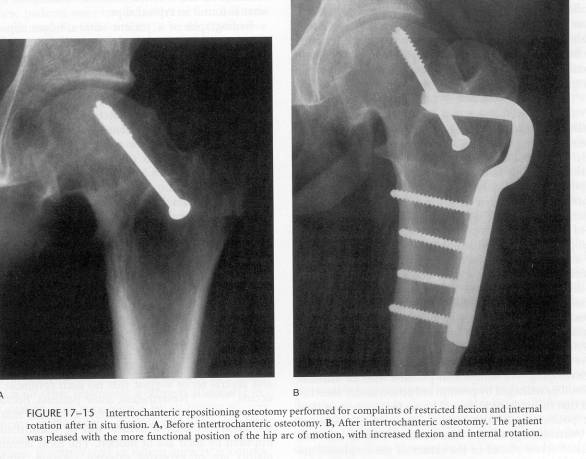
Degenerative osteoarthritis , decreased ROM and persistent out-toeing are all common long term problems, especially in moderate and severe slips. Various osteotomies from base of the femoral neck to the Southwick trochanteric level osteotomies have been suggested for treatment. These are complex and difficult osteotomies, often with high complication rates.
Therefore the best treatment for SCFE is early treatment before severe displacement or instability of the physis occurs.