Fractures of the Femur
Proximal Femur Fractures
Hip fractures in children are of interest because of the frequency of complications rather than the frequency of the fractures. Hip fractures in children are rare compared to hip fractures in adults with osteoporotic bone, and the fracture patterns and classification are different.
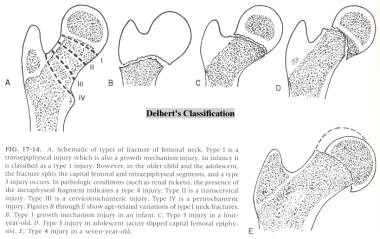
Unlike hip fractures in adults, almost all hip fractures in children are caused by severe trauma. In four large series, 75% to 80% occurred from severe trauma. The femoral neck in children, except for the proximal femoral physis, is extremely strong. High-velocity forces, like those absorbed in motor vehicle accidents and high falls are necessary to cause these fractures. Delbert’s classification is often used to describe these injuries (see figure 17-14 below ).
The three main complications encountered when treating pediatric hip fractures are nonunion, physeal injury and osseosnecrosis. These three occur in differing frequencies depending upon the Delbert type of the fracture.
To understand osseosnecrosis, the blood supply of the femoral head must be understood. The vessels of the ligamentum teres are of virtually no importance. At birth, the branches of the medial and lateral circumflex arteries (metaphyseal vessels) traversing the femoral neck predominately supply the femoral head. These arteries gradually diminish in size as the cartilaginous physis develops and forms a barrier that prevents penetration of these vessels into the femoral head. This metaphyseal blood supply is virtually nonexistent by age 4. When the metaphyseal vessels diminish, the lateral epiphyseal vessels predominate, and the femoral head is primarily supplied by these vessels, which bypass the physeal barrier. At about age 3 to 4, the lateral posterosuperior vessels appear to predominate and to supply all the anterior lateral portion of the head of the femoral epiphysis. The posteroinferior and posterosuperior arteries persist throughout life and supply the femoral head.
Delbet’s classification is often used, and is divided into four types based on anatomic location of the fracture.
Transepiphyseal fractures (type I) occur through the proximal femoral physis. In children, severe violence is necessary to produce this separation, and in infants it can be caused by child abuse. In adolescents, however, less trauma may be necessary because it may represent one end of the spectrum of slipped capital femoral epiphysis. It may also occur as a pathologic separation associated with renal osteodystrophy, hypothyroidism, or neglected septic arthritis. Transepiphyseal fractures represent about 8% of all hip fractures in children. Dislocation of the femoral head occurs in 50%, osseosnecrosis in 80-100% and physeal growth arrest in 80-100%.
When a transepiphyseal fracture is displaced but not dislocated, treatment algorithms vary by institution. In general, it seems that a logical approach includes attempts at gentle closed reduction with a low threshold for opening if redisplacement occurs or appears to become inevitable. Smooth pin fixation has been advocated to avoid further physeal injury should opening become necessary. In either case, spica casting seems to be the accepted method of immobilization.
Transepiphyseal separations with dislocation of the femoral head almost always require open reduction and almost always have poor results. One reason cited is that the diagnosis and treatment often are missed or delayed because of concomitant injuries.
Transcervical fractures (type II) account for the greatest percentage (45% to 50%) of hip fractures in children. This fracture, especially if not significantly displaced, may appear innocuous on x-rays; however, the avascular necrosis rate may be as high as 50%. This can be significantly higher than the reported 15-40% rates in similar adult fractures, and is probably due to the tenuous, changing blood supply to the proximal femoral epiphysis in children. Although this has not been totally substantiated, compromise of the blood supply may occur at the moment of maximum displacement of the fracture at the time of the injury.
The occurrence of other complications, including loss of reduction and resultant coxa vara (20%), premature physeal closure, and nonunion, may be influenced by the type of treatment, more so than the amount of displacement, which has been shown to be most predictive of osseous necrosis. Stable fracture fixation takes precedence over preservation of the physis, especially in type II fractures in children older than age 8 years.
Cervicotrochanteric fractures (type III) are the second most common type of hip fractures in children. Unfortunately, regardless of the type of treatment, avascular necrosis occurs in 20-30% of children with cervicotrochanteric fractures, particularly those that are displaced.
Displaced cervicotrochanteric fractures are similar to transcervical fractures in regard to the development of complications; undisplaced cervicotrochanteric fractures are similar to intertrochanteric fractures, with fewer complications.
Treatment of displaced cervicotrochanteric fractures is controversial, due to the risks of osseous necrosis and the late coxa vara deformity that occurs in approximately 20% of cases. If a nondisplaced cervicotrochanteric fracture is treated by abduction spica casting, close follow-up with frequent x-rays is necessary to note any displacement in the cast and to avoid a coxa vara deformity. If displacement occurs, immediate reduction and internal fixation are indicated.
Intertrochanteric fractures (type IV) in children usually are caused by falls or being struck by a moving vehicle. The fracture is far less common than transcervical and cervicotrochanteric fractures. This fracture has far fewer complications than any of the other three types, with a reported osseosnecrosis rate of about 10% and a coxa vara deformity occurring in 10-15%. This fracture is often comminuted, but because of a child’s osteogenic potential, nonunion almost never occurs. An acceptable position can usually be obtained in very young children by skin or skeletal traction, followed by an abduction spica cast. Occasionally, if the fracture cannot be reduced with traction, gentle closed manipulation can be used. When internal fixation becomes necessary, a combination screw and side plate device should be used, avoiding the proximal femoral physis and the greater trochanteric apophysis if possible.
Femoral Shaft Fractures
Femoral shaft fractures, including subtrochanteric and supracondylar fractures, represent approximately 2% of all bony injuries in children. The male-to-female ratio of femoral fracture is 2.6:1 with a bimodal distribution. The first peak occurs in early childhood, the second in mid-adolescence. Although femoral shaft fractures are dramatic and disabling injuries both to the patient and the family, most unite rapidly without significant complications or sequelae.
In early childhood, the femur is relatively weak and can break under load conditions reached in normal play. In adolescence, high-velocity trauma is required to reach the stresses necessary for fracture. In children younger than walking age, up to 80% of femoral fractures are caused by abuse, as are 30% in children younger than 4 years of age. In older children, femoral fractures are most likely to be caused by high-energy injuries, such as motor vehicle accidents, which account for over 90% of femoral fractures in this age group.
Femoral fractures are classified as (1) transverse, spiral, or oblique; (2) comminuted or noncomminuted; and (3) open or closed. Open fractures are classified according to Gustilo’s system. The presence or absence of vascular and neurologic injury is documented and is part of the description of the fracture. The most common femoral fracture in children (over 50%) is a simple transverse, closed, noncomminuted injury.
The level of the fracture leads to characteristic displacement of the fragments based on the attached muscles. With subtrochanteric fractures, the proximal fragment lies in abduction, flexion, and external rotation. The pull of the gastrocnemius on the distal fragment in a supracondylar fracture produces an extension deformity, which may make the femur difficult to align.
Treatment of femoral shaft fractures in children is age dependent, with considerable overlap between age groups. The child’s size and bone age also must be considered, as well as the cause of the injury. Whether the femoral fracture is an isolated injury or part of polytrauma influences treatment choices
In infants, newborn to 6 months of age, femoral fractures usually are stable because of the thick periosteum. For stable proximal or mid-shaft femoral fractures, simple splinting or a Pavlik harness is all that is required. For femoral fractures with excessive shortening (more than 1 to 2 cm) or angulation (more than 30°), spica casting is required. Traction is rarely necessary in this age group. A skeletal survey should be completed in these cases, as there is a high rate of association with child abuse.
In children between the ages of 6 months and 6 years, immediate or early spica casting is the treatment of choice for femoral fractures with less than 2 cm of initial shortening. Femoral fractures with more than 2 cm of initial shortening or marked instability and fractures that cannot be reduced with immediate spica casting require 3 to 10 days of skin or skeletal traction. Skeletal stabilization by external fixation is reserved for children with open fractures or multiple trauma. Intramedullary rodding is used only in children with metabolic bone disease that predisposes to fracture or after multiple fractures, such as in osteogenesis imperfecta.
Treatment of femoral fractures in children between 6 and 11 years of age is controversial. Although spica casting with or without internal fixation can be used, children greater than 60 pounds are very difficult to care for in a spica cast. Because of the cost and the social problems that may accompany management of a child in a spica cast, enthusiasm for skeletal fixation has increased in recent years. Skeletal fixation is frequently used in children with multiple trauma, head injury, vascular compromise, “floating knee” injuries, or multiple fractures. Treatment options should be discussed with the parents before choosing the method of fracture fixation. Fixation methods include; open reduction and fixation with a small plate and placement of a spica cast (though plating can lead to significant overgrowth phenomenon, and subsequent limb length discrepancy), external fixator application or the use of flexible intramedullary rods (such as Enders nails or rush rods).
Standard rigid intramedullary rod fixation may not be appropriate for femoral fractures in children from 12 years of age to maturity, due to increased risk osseous necrosis of the femoral head. Most surgeons will base implant selection on the radiographically determined skeletal age of the patient, treating younger appearing individuals with flexible rods, and older appearing individuals with rigid rods.
In general, considering all methods of treatment, femur fractures do very well. Complications such as shortening and angular deformity usually result from poor attention to detail. Close follow-up and timely interventions (if needed) should allow adequate healing, whichever method is chosen. Overgrowth phenomenon can be expected. Reports show an average lifetime overgrowth of 1.6 cm for a child’s femur that has sustained a shaft fracture. As is intuitively evident, this overgrowth is generally inversely proportional to the skeletal age at which the fracture is sustained.
Fractures About the Knee
Distal Femoral Fractures
Distal femoral epiphyseal fractures are typically of two types; hyperflexion or varus-valgus. In hyperextension type fractures, the epiphysis is displaced anteriorly and the metaphysis is displaced into the popliteal fossa, making neurovascular injury possible. Reduction often is unstable because extreme knee flexion may be required to tighten the anterior soft-tissue hinge. Varus–valgus fractures result from an abduction or adduction force, and the posterior periosteal hinge is intact. In either type of fracture, reduction must be precise because any residual varus or valgus about the knee has limited remodeling potential.
Distal femoral physeal injuries account for 1% to 6% of all physeal injuries and for fewer than 1% of all fractures in children. They are much less common than physeal injuries of the ankle or upper extremity. Most are Salter-Harris type II injuries. Although separations through the cartilaginous physis would seem to be more likely than fractures through the hard cortical bone of the femoral shaft, the physis is protected by its large surface area and its undulating shape. These same properties however may contribute to the growth disturbance that can often occur after Salter-Harris type I distal femoral injuries, contrary to the usual expectations for most Salter-Harris type I fractures.
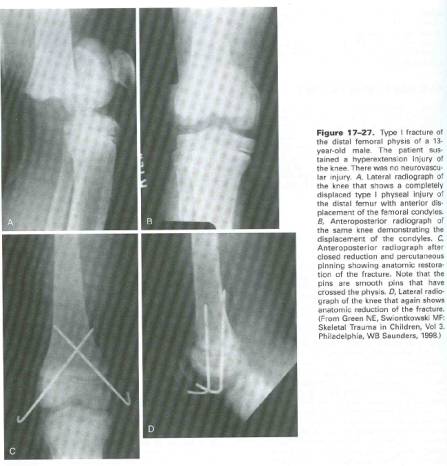
Many clinical studies of distal femoral physeal fractures show a high incidence of physeal growth disturbance, resulting in asymmetry of length, angulation, or both. Growth disturbance is caused by bony bridging resulting from direct physeal trauma or from lack of anatomic reduction of the physis. Some authors believe that the likelihood of physeal disturbance increases with increasing degrees of initial displacement of the fracture. The complex contour of the physis makes it possible for shearing of the fracture line to occur across the physis, even in some “benign” fracture patterns such as Salter-Harris type I and II injuries.
These injuries can at times be challenging to diagnose with standard orthogonal views. Oblique views of the distal femur may reveal an occult fracture through the epiphysis or metaphysis. Stress x-ray views should be considered if multiple plain films are negative in a patient with tenderness localized to the physis or an effusion
The Salter-Harris type II pattern, characterized by an oblique extension of the fracture across one corner of the adjacent metaphysis, is the most common type of separation at the distal femur and usually occurs in adolescents. Displacement is usually toward the side of the metaphyseal fragment. The incidence of premature growth arrest, even with satisfactory reduction, is high due to the energy required to create this injury and the undulating morphology of the distal femoral physis. If asymmetric growth follows a type II separation, the portion of the physis underneath the metaphyseal fracture usually is spared. Therefore, if the metaphyseal fracture is medial, deformity is more likely to be valgus than varus. If the metaphyseal fracture is lateral, varus angulation is more likely.
Salter-Harris type III distal femoral injuries usually have the epiphyseal fracture line within the intercondylar notch. Salter-Harris type III injuries most often are caused by valgus stress in sports and usually involve the medial condyle. The fracture may be nondisplaced and detected only with a stress x-ray. If displaced, reduction usually is unstable and requires internal fixation. A displaced type III fracture may cause incongruity of the joint surface, especially of the patellofemoral articulation.
Salter-Harris type IV injuries of the distal femur are uncommon. A vertical fracture line extends from the metaphyseal cortex down across the physis and enters the articular surface of the epiphysis. Even slight displacement of the fracture fragment may produce growth disturbance from formation of a bony bridge from the displaced epiphysis to the metaphysis. Therefore, anatomic reduction and internal fixation are advised.
Salter-Harris type V injuries are rare. Most commonly, the diagnosis is made in retrospect at the time of evaluation for premature growth arrest and limb-length discrepancy or angular deformity.
Even less common is an avulsion injury to the edge of the physis. A small fragment, including a portion of the perichondrium and underlying bone, may be torn off when the proximal attachment of the collateral ligament is avulsed. This uncommon injury may also lead to localized premature growth arrest and progressive angular deformity. The bony bridge usually is small, localized, and surgically accessible, and excision is appropriate.
Anatomic reduction of a displaced separation of the distal femoral epiphysis is desirable, and the closer the patient is to skeletal maturity, the greater the need for exact realignment. Residual varus or valgus deformity after failure to obtain complete reduction usually does not remodel with further growth. Reduction of displacement in the sagittal plane may be slightly less precise.
Closed reduction may fail for a number of reasons, making open reduction necessary. A Salter-Harris type I or II separation may be irreducible by closed methods because of interposed soft tissue, usually a flap of torn periosteum or muscle that curls up inside the separation cleft. Displaced Salter-Harris type III or IV separations almost always require open reduction and internal fixation to minimize disruption of the articular surface and to decrease the likelihood of premature growth arrest. In an open injury, open reduction and fixation may be accomplished at the time of wound debridement. Whenever possible, fixation devices are placed to avoid crossing the physis.
At the time of initial evaluation and treatment planning, the short-and long-term problems and complications are explained to the patient and parents. The need for long-term follow-up is stressed from the beginning of treatment.
Proximal Tibial Physeal Fractures
The physis of the proximal tibia is well protected in contrast to the distal femoral physis. On the lateral aspect, the proximal tibial epiphysis is buttressed by the upper end of the fibula. Anteriorly, the tubercle projects down from the epiphysis to overhang the adjacent metaphysis. The superficial portion of the medial collateral ligament inserts beyond the physis into the upper metaphysis. In the posteromedial corner, the insertion of the semimembranosus muscle spans the physis. Thus, there is nearly circumferential reinforcement to the perichondrium. Because of this protection, separation of the proximal tibial epiphysis is relatively rare.
Fracture–separation of the proximal tibial epiphysis can be caused by a direct or indirect force. Most often, it is caused by the indirect mechanism of the lower leg being forced into abduction or hyperextension against the fixed knee.
The most serious complication of injury to the proximal tibia is vascular compromise. The popliteal artery is tethered by its trifurcation near the posterior surface of the proximal tibial epiphysis. The posterior tibial branch passes under the arching fibers of the soleus. The anterior tibial artery passes forward through an aperture above the proximal border of the interosseous membrane. A hyperextension injury that results in posterior displacement of the upper end of the metaphysis may stretch and tear the bound popliteal artery.
As such is the case, vascular status must be carefully documented.
Most separations of the proximal tibial epiphysis are Salter-Harris type I and II injuries . A patient with a separation of the proximal tibial epiphysis usually has a knee joint tense with hemarthrosis and extension is limited because of hamstring spasm. Typically, tenderness is present over the proximal tibial physis. A small bony fragment at the periphery of the metaphysis may be the only radiographic clue to the diagnosis. Fracture lines may be visible only on oblique x-rays.
Hyperextension fractures are reduced with a longitudinal force on the tibia combined with a gentle, anterior translating force on the proximal metaphysis. Counter traction on the femoral shaft is applied by an assistant. An above knee cast is applied after reduction is obtained.
An abduction fracture with valgus angulation usually can be reduced by adducting the leg on the extended knee. This should be a gentle manipulation to decrease the risk of injury to the peroneal nerve. After reduction, a long-leg cast with varus molding is applied with the knee in slight flexion.
Separations of the proximal tibial epiphysis may be surprisingly unstable. Smooth pins may be inserted percutaneously, crossing distal to the physis to maintain reduction. The proximal ends should not protrude into the knee joint. An image intensifier makes percutaneous fixation easier.
Open reduction is indicated for displaced Salter Harris type III injuries. An anterior incision is used to allow inspection of the articular surface. A pin is inserted in the displaced fragment and is used to guide it toward reduction. Other pins or screws are then inserted horizontally across the epiphysis.
Tibial Shaft injuries
Tibial and fibular fractures are the third most common pediatric long bone injuries (15%) after femoral and radial and ulnar fractures. Thirty percent of tibial fractures in children occur with concomitant ipsilateral fibular fractures. About 50% occur in the distal third of the tibia, 39% in the middle third. About 35% of tibial fractures in children are oblique, 32% are comminuted, 20% are transverse, and 13% are spiral.
Fractures of the diaphysis and the metaphysis of the tibia often result from indirect forces applied to the lower extremity. Direct trauma usually produces a transverse or a comminuted fracture. Rotational forces produce an oblique or a spiral fracture.
Nonphyseal injuries of the tibia and the fibula can be classified into three major categories based on the combination of bones fractured and the location of the injuries; Fractures of the proximal tibial metaphysis, diaphyseal fractures and fractures of the distal tibial metaphysis.
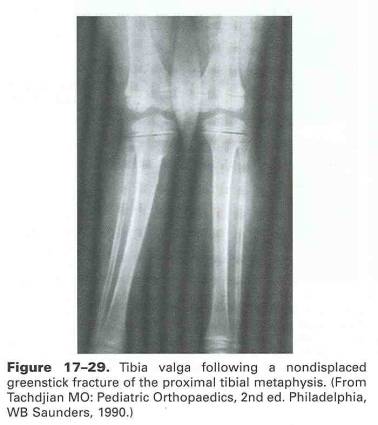
Fractures of the proximal tibial metaphysis usually occur in children ages 3 to 6 years. The most common mechanism of injury nationwide is a force applied to the lateral aspect of the extended knee that causes the cortex of the medial metaphysis to fail in tension. Here in Utah, anecdotally speaking, the great majority of these valgus mechanism proximal tibial metaphyseal injuries are caused by trampoline related incidents. The fracture may be complete or greenstick. The fibula usually is not fractured, although plastic deformation occasionally occurs.
Nondisplaced proximal metaphyseal tibial fractures are stabilized with a long-leg cast in 10° flexion. Displaced proximal tibial fractures are reduced closed with the patient under general anesthesia. Fluoroscopy is used to verify an anatomic reduction. Fractures that cannot be reduced closed require open reduction, with removal of interposed soft tissue from the fracture and repair of the pes anserinus insertion if necessary.
The most common sequela after proximal tibial metaphyseal fractures is a late valgus deformity, known as Cozen’s phenomenon (figure 17-29). A child with a post-traumatic valgus deformity should be followed until spontaneous correction occurs or until adolescence. Proximal tibial osteotomy is not favored due to the high incidence of overgrowth, and recreation of the valgus deformity in 80% of cases. A carefully planned proximal tibial medial epiphysiodesis performed in early adolescence should provide results better than those of osteotomy without many of the risks. Proximal tibial osteotomy is recommended in adolescents near skeletal maturity if hemiepiphysiodesis is not an option. Orthotic devices have not been shown to alter the natural history of post-traumatic valgus deformity of the tibia.
Most tibial and fibular shaft fractures in children are uncomplicated and can be treated by a simple manipulation and cast application. The surgeon should be cautious to rule out compartment syndrome, and should admit injuries of this nature for close surveillance. Initially splinting is most appropriate to allow for anticipated swelling, and can be followed by casting in 5-10 days. Varus malalignment often develops after isolated tibial shaft fractures, and valgus angulation, recurvatum, and shortening can be significant problems with complete fractures of both the tibia and fibula
Displaced fractures may be reduced in the operating room to allow painless manipulation with muscle relaxation and the use of fluoroscopy to guide the reduction. The fracture is evaluated under fluoroscopy to determine the most appropriate way to manipulate the bone to achieve an acceptable alignment. The goal is to obtain at least 50% apposition of the tibia and alignment within 5° to 10° of normal in all planes. A long-leg cast is applied with the ankle left in mild plantarflexion during the initial 2 to 3 weeks to prevent posterior angulation at the fracture.
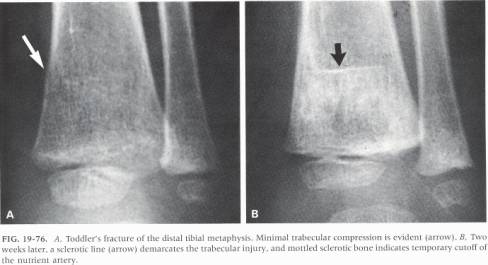
Another entity, known as a toddler’s fracture can be seen in the distal metaphysis of the tibia. This is an impaction type injury that is usually initially diagnosed clinically, then confirmed when radiographic healing becomes evident 10 days or so later (see figure 19-76 below). Treatement involves prevention of further injury with casting.
Most children with unstable tibial fractures are placed in a bent-knee (45°) above knee cast. This controls rotation at the fracture and helps keep the child non-weight-bearing during the initial healing phase. The alignment of the fracture must be monitored closely during the first 3 weeks after the cast has been applied, because muscle atrophy and a reduction in tissue edema may cause a loss of reduction that occasionally results in malalignment of the fracture. Some children require a second cast application with the use of general anesthesia 2 to 3 weeks after injury to realign the fracture.
Stable fractures and minimally displaced fractures should be treated closed whenever possible, but unstable fractures of the tibia and fibula may require operative reduction and stabilization, especially in older adolescents. Methods of fixation include percutaneous pins, external fixation, plates and screws, and intramedullary nails.
Indications for operative stabilization of tibial fractures in young children are few. Comminuted tibial fractures, irreducible fractures, fractures that cannot be maintained in a reduced position, fractures associated with a compartment syndrome, and grade II or III open injuries should be treated with operative stabilization. Other indications for operative treatment of the fractures in children include spasticity and fractures in which open treatment facilitates overall care.
Fractures of the distal tibial metaphysis are often greenstick injuries. The anterior cortex is impacted, the posterior cortex is fractured completely, and the overlying periosteum is torn, often resulting in a recurvatum deformity. Reduction should be performed with the use of general anesthesia. An above knee cast is applied with the foot in plantarflexion to prevent recurvatum. The foot is brought up after 3 to 4 weeks of immobilization and a short-leg walking cast is applied. Unstable injuries can be fixed with pins
Complications are rare in the treatment of pediatric tibial fractures, but can be devastating. Some entities to look out for include compartment syndrome, vascular injury, neurologic injury, malrotation, angular deformities, proximal tibial physeal closure, leg-length discrepancy, delayed union and non-union.
Ankle Injuries
Typically, pediatric ankle injuries involve the distal tibial physeal plate. Growth arrest is therefore a significant complication that should be anticipated and managed. Generally, partial arrest and angular deformity are the rule, but complete arrest and subsequent leg length discrepancy have been known to occur as well.
In children, all of the ligamentous structures that bind the medial and lateral malleolae to the talus and the distal tibial epiphysis to the distal fibular epiphysis are attached to the malleolae distal to the physes. Because the ligaments are stronger than the physes, physeal fractures are more common than ligamentous injuries in children
Pediatric ankle fractures can be classified either by anatomic description, or by using the Dias-Tachdjian modification of the adult-use Lauge-Hansen classification. This second method focuses on the mechanism of fracture formation. Though it is commonly used, it has relatively poor intra-observer reliability, and will therefore not be discussed herein. There are however, a few specific fractures that are unique to the pediatric patient that should be understood and carefully ruled out in the injured child.
First is the juvenile Tillaux fracture (see figure 19-105 below). It is a Salter-Harris type III fracture involving the anterolateral distal tibia. The portion of the physis not involved in the fracture is closed. Second is the “triplane” fracture, which describes a fracture that has the appearance of a Salter-Harris type III fracture on the anteroposterior x-ray and of a Salter-Harris type II fracture on the lateral x-ray. Collectively, these two fracture types are known as “transitional” fractures, because they occur through a physis that is in a position of closing. The distal tibial physis closes from posteromedial to anterolateral, leaving that anterolateral physeal region susceptible to the insults causative of Tillaux and triplane fractures.
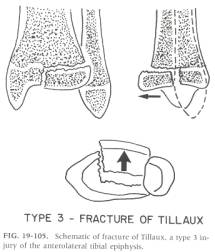
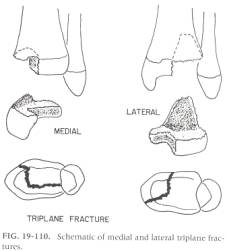
Appropriate treatment of ankle fractures in children depends on the location of the fracture, the degree of displacement, and the age of the child. Nondisplaced fractures may be simply immobilized. Both below-knee and above-knee casts have been used for immobilization of nondisplaced juvenile Tillaux and triplane fractures. Closed reduction and cast immobilization may be appropriate for displaced fractures. If the closed reduction cannot be maintained with casting, percutaneous or external skeletal fixation may be necessary. If closed reduction is not possible, open reduction may be indicated, followed by internal fixation or cast immobilization. As always, great care should be paid to the quality of the articular reduction, and whenever possible, the physes should not be violated with hardware. If the physes must be violated, smooth pin fixation is preferred.
Foot Injuries
The diagnosis and treatment of foot injuries in the child are remarkably similar to their adult counterparts. It is sometimes, however, difficult to differentiate between relatively minor injuries and the multitude of sesamoids and minor growth variants in the growing foot. A careful review of radiographs is a must to avoid mistaking injury for anatomy, and vice-versa.
The newborn foot is extremely pliable, and foot injuries in early childhood are extremely unusual. Exceptions are major vehicular injuries, lawn mower injuries, and snowmobile injuries. As the foot becomes more ossified during childhood, fractures occur more regularly, but significant injuries are still unusual.
Forefoot injuries (fractures of the metatarsals and phalanges) are almost always treated non-operatively, and excellent results can typically be expected.
Midfoot injuries are typically to the ligament connecting the first cuneiform to the base of the second metatarsal. This is known as Lisfranc’s ligament, and can be injured by forced plantar flexion with or without a rotational component. Bunk bed injuries are also seen from time to time, where a fall from such a height may result in and epiphyseal injury to either the base of the first metatarsal, or the distal aspect of the first cuneiform. Treatment is closed for minimally displaced injuries, closed with percutaneous pinning for displaced but reducible injuries and open for irreducible injuries.
Hindfoot fractures (talus and calcaneus) are of far less severity in children owing to the increased resilience of these largely cartilaginous structures. These fractures are often missed on initial radiographs, and become evident after 10-14 days of healing. Talar neck fractures are caused by forced dorsiflexion, and like their adult equivalent should be treated aggressively, as osseous necrosis can and does occur. Subsequent talar flattening and ankle stiffness will result. Calcaneus fractures typically can be treated closed, but may sometimes require surgery to restore articular alignment. Subtalar dislocations are rare, and therefore frequently overlooked. When diagnosed early, closed treatment is usually successful, but when missed initially may require open reduction and temporary transarticular fixation.

