There are certain inherent mechanical and biologic differences between the child and the adult that the treating physician must consider when selecting appropriate treatment, and when providing the patient and family with prognostic information.
Mechanically speaking, children differ from adults in that their bone exhibits a much higher degree of elasticity. Long bones in particular show a much higher propensity for plastic deformation, with or without completion of the fracture. Torus, or (“buckle”) fractures and “Greenstick” fractures are a good example of such deformation, without fracture completion.
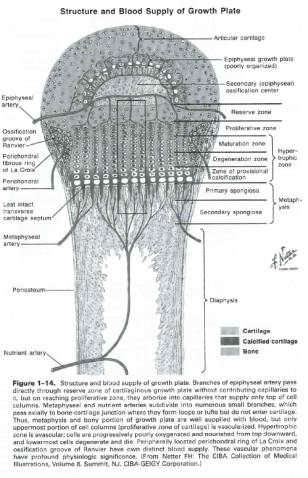
Equally important is the relative stiffness of pediatric bone vs. adjacent and supporting soft tissue structures such as ligaments. Given the inherent weakness of the physis, or growth plate, the pediatric musculoskeletal construct is far more likely to fail at the physis, rather than through surrounding ligaments. The physis is made up of four layers of varying stiffness, and fracture will occur between stiff and weaker layers. Most commonly failure occurs through the hypertrophic zone of cartilage (see fig. 1-4).
Fractures at or about the physis are generally classified using the Salter-Harris schema. Occasionally, stress views, or more advanced imaging procedures such as MRI are required to make the diagnosis. Remember, ligament sprains and strains are rare in children. When faced with a scenario of laxity about a child’s joint, it is imperative to rule out the presence of a physeal injury or periarticular fracture.
The increased level of activity observed in children can work both for and against the treating physician. On one hand, increased activity will allow better post-immobilization rehabilitation, and faster return to normal function, whereas on the other hand, the child will be at increased risk for re-injury following premature removal of immobilizing restraints.
Biologically, children differ from adults in several key ways. First, they are undergoing a process of active skeletal growth. Remodeling potential must therefore be considered when determining appropriate treatment. Ordinarily, remodeling potential will work to the advantage of the treating surgeon. This will allow greater tolerance for incomplete reduction including; increased displacement, greater angulation, and/or some degree of overriding. Rotational malalignment is however not as readily amenable to remodeling and should be avoided.
Furthermore, unlike the thin fibrous adult periosteum, the pediatric periosteum is quite thick, very vascular and highly osteogenic. It contains both an outer fibrous layer, and an inner cambium, or osteogenic, layer. This periosteum is crucial in preventing significant displacement at the time of injury, and can often provide useful assistance in obtaining a satisfactory reduction. This stout layer is also therefore capable of becoming interposed between fracture ends and preventing adequate reduction.
In general, there is believed to be a richer blood supply to the bone of the growing child, when compared to that of adults. This contributes to more rapid healing, and bony union. It is however important to note that children, like adults, are susceptible to avascularity in certain regions, such as the femoral head and the lateral condyle of the distal humerus.
Though, these biologic and mechanical differences generally work toward improving outcomes in the child, there are certain complications that are unique in this population that are not observed in the adult population. First, growth plate arrest can be a challenge in treatment. Arrest can be complete, leading to limb length discrepancy, or partial, leading to angular deformity. The degree to which each of these complications is likely to occur can be estimated given the particular type of Salter-Harris injury observed. Moreover, growth stimulation can also be challenging, and can lead to limb length discrepancy by virtue of overgrowth of the affected limb. This is particularly common in healing fractures of the femoral shaft. It is imperative that the skeletal age of the patient be assessed, so that the remodeling potential can be predicted. Occasionally, fractures in children approaching skeletal maturity can be treated as if the patient were in fact an adult.