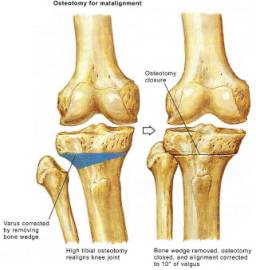
Realignment osteotomies are based on the assumption that excessive force carried across the joint from abnormal limb alignment leads to accelerated degeneration within the affected joint or joint compartment. Cadaveric models have demonstrated increased contact pressures in knees that undergo varus or valgus malalignment of the tibia. With time, the excessive pressure leads to breakdown of the cartilage matrix and ultimately loss of structural integrity. In the medial compartment of the knee, (Figure 43) for example, once arthritis is clinically established, serial examinations showed a clinical and radiographic progression of DJD in nearly all cases. Knees with a valgus mal alignment can also have isolated lateral compartment disease analogous to the degenerative varus knee. The goal of any realignment osteotomy is to alter the loading forces across the knee to unload the affected compartment, and thereby to gain relief of pain and slow degenerative progression.
Normally, sixty percent of an individual’s body weight passes through the medial compartment of the knee. Loads up to 4 times body weight are produced in this area while climbing stairs. This differential loading often contributes to most common deformity seen in DJD of the knee, the varus knee. Valgus osteotomies can redistribute these forces and mitigate rapid further joint destruction. Patient selection is crucial to the success of this procedure. The valgus osteotomy is indicated in patients that have uni-compartmental disease, have a physiologic age < 60 yrs, are not obese (> 80 kg are at increased risk for component failure), have a good preoperative range of motion (range of motion is not likely to improve with an osteotomy), and have an active occupation or lifestyle which they want to maintain. A patient’s angular deformity should have the following parameters: 1)> 15 deg of fixed varus deformity (often patients will have varus laxity) 2)< 15 degrees flexion contracture 3)> 90 degrees flexion. A patient should obviously have radiographically intact lateral and patellofemoral compartments. Any symptoms in these compartments will not be treated with a valgus osteotomy.
Contraindications are many and include a) Lateral tibial Subluxation > 1 cm b) rheumatoid arthritis and other inflammatory arthropathies c) presence of an ACL tear and d) osteochondral injuries with involvement of more than 1/3 the condylar surface or OCD lesion that is more than 5 mm deep e) medial compartment bone loss of more than 2-3mm f) flexion contracture of more than 15º, g)knee flexion less than 90º, h) more than 20º of correction needed and i)more than one compartment with DJD. The most significant contraindication to valgus-producing osteotomy is symptomatic or radiographic arthritis in one or both of the other joint compartments. In addition, a relative contraindication is a knee that has a varus thrust. Optimum results are obtained when over correction of 8-10º valgus is obtained in a patient that is not overweight. Furthermore, the procedure, by design, results in valgus alignment of the lower extremity, which may be unacceptable to some patients cosmetically.
Figure 44
Figure 45
Lateral Compartment Disease can also be treated with osteotomy. If < 12 degrees valgus deformity is present than a varus producing proximal tibial osteotomy should be performed. However, if >12 degrees valgus is present than the plane of the joint line deviates significantly from the horizontal and a medial closing wedge osteotomy of distal femur (supracondylar) is preferred. This procedure should ideally restore a horizontal joint line and a tibiofemoral angle of 0º. When a supracondylar femur osteotomy is later converted to a TKA, restoring the desired anatomical valgus through the distal femoral cuts is often very difficult.
Isolated medial compartment disease is treated with a high tibial osteotomy (HTO) or above the tibial tubercle. (Figure 45) The most common technique is a lateral closing wedge & fibular shortening. Overcorrection of the mechanical axis by an additional 3º of valgus over the normal 7º is ideal. Complications include: 1) Undercorrection – most common 2) Overcorrection 3) Penetration of the articular surface 4) AVN of tibial plateau 5) Patella baja 6)Peroneal nerve injury 7) Anterior compartment syndrome 8) TKR may be more difficult
PITFALLS AND COMPLICATIONS
Reliable good results from HTO have been reported for up to 10 years after surgery. However, failures increase with time owing to progression of arthritis into the remaining joint compartments or recurrence of varus deformity. Patients can anticipate 8 to 10 years of pain relief following tibial osteotomy if ideal patient selection is held to, and bony union obtained. The most common complication is nonunion of the osteotomy. Nonunion can be avoided by ensuring that the osteotomy is rigidly fixed with good impaction of the bone fragments. If residual motion is evident after fixation, consider additional fixation such as an anteroposterior interfragmentary screw or a smaller supplementary plate. Avoid stiffness of the knee by early motion, supervised, if necessary, by a therapist to be certain that the patient regains motion. Failed HTO is best addressed with total knee arthroplasty. Unfortunately, proximal tibia osteotomy can compromise the almost inevitable total knee arthroplasty. Patients who have had a prior HTO with subsequent TKA are more likely to have pain post TKA than matched controls. Patella baja, lateral soft-tissue scarring, and abnormal proximal tibia anatomy are all technical challenges encountered when performing arthroplasty subsequent to HTO. These considerations should be discussed with a patient when advising patients who are considering tibial osteotomy.